In continuation of my update on Ketamine

Advancing the understanding and treatment of psychiatric disorders is
a principal goal of neuroscientists. As mental disorders are the
leading cause of disabilities worldwide, it is concerning that there are
few effective therapeutics on the market due to the lack of knowledge
regarding pathophysiology. In particular, the main treatment for major
depressive disorders are antidepressants, which target the monoaminergic
system and include selective serotonin reuptake inhibitors (SSRIs).
However, these drugs take six weeks on average before symptom relief and
many individuals are unaffected by them.
a principal goal of neuroscientists. As mental disorders are the
leading cause of disabilities worldwide, it is concerning that there are
few effective therapeutics on the market due to the lack of knowledge
regarding pathophysiology. In particular, the main treatment for major
depressive disorders are antidepressants, which target the monoaminergic
system and include selective serotonin reuptake inhibitors (SSRIs).
However, these drugs take six weeks on average before symptom relief and
many individuals are unaffected by them.
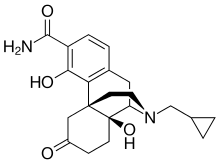
Ketamine, a synthetic analogue of PCP, has recently taken the
spotlight as a novel, fast-acting antidepressant. The benefits of
ketamine include a one-time, low-dose IV infusion, where symptoms are
alleviated within hours and which lasts for up to two weeks in patients
with depression. Even more compelling is that this regimen affects
patients with treatment-resistant depression, meaning those who do not
respond to current antidepressants. These effects are especially
important in helping individuals with depression who may be experiencing
suicidal ideation because of ketamine's fast-acting nature and it is
the only treatment effective for treatment resistant patients.
However, there are many downsides to the use of ketamine as an
antidepressant, especially with long-term or repeated use. For example,
ketamine is an illicit drug with high abuse potential, commonly known as
the party drug "Special K." Therefore, close clinical monitoring of the
use of this drug is necessary. In regards to neuroscience research in
the past decade, it has been demonstrated that chronic, low-dose
ketamine has been used to study learning and memory deficits in a rodent
model of schizophrenia. The biochemical data from these animals reveal a
change in a specific type of neuron in the brain that is important for
network activity underlying normal cognitive functioning. This begs the
question: Can ketamine work as an antidepressant without producing
cognitive deficits associated long-term use?
antidepressant, especially with long-term or repeated use. For example,
ketamine is an illicit drug with high abuse potential, commonly known as
the party drug "Special K." Therefore, close clinical monitoring of the
use of this drug is necessary. In regards to neuroscience research in
the past decade, it has been demonstrated that chronic, low-dose
ketamine has been used to study learning and memory deficits in a rodent
model of schizophrenia. The biochemical data from these animals reveal a
change in a specific type of neuron in the brain that is important for
network activity underlying normal cognitive functioning. This begs the
question: Can ketamine work as an antidepressant without producing
cognitive deficits associated long-term use?
In order to address this question, we need to understand the molecular
mechanisms that ketamine is utilizing to produce these beneficial
antidepressant effects. Although researchers do not know exactly how
ketamine works, we know that it is in a different way than current
antidepressants on the market. There is no clear answer yet, but researchers have produced some promising results. Using ketamine to
deepen our understanding of depression will advance the field of neuroscience and ultimately lead to a more effective treatment for the disorder.
mechanisms that ketamine is utilizing to produce these beneficial
antidepressant effects. Although researchers do not know exactly how
ketamine works, we know that it is in a different way than current
antidepressants on the market. There is no clear answer yet, but researchers have produced some promising results. Using ketamine to
deepen our understanding of depression will advance the field of neuroscience and ultimately lead to a more effective treatment for the disorder.