In continuation of my update on methylphenidate
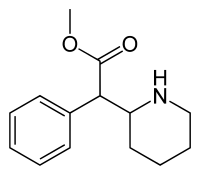
Adlon Therapeutics L.P., a subsidiary of Purdue Pharma L.P., announced that the U.S. Food and Drug Administration (FDA) approved Adhansia XR (methylphenidate hydrochloride) extended-release capsules CII, a central nervous system (CNS) stimulant, for the treatment of Attention-Deficit/Hyperactivity Disorder (ADHD) in patients six years and older. In a simulated Adult Workplace Environment (AWE) study, Adhansia XR demonstrated statistically significant improvement over placebo at 1, 2, 5, 8, 11, and 16 hours post-dose, but not at hour 14 post-dose.1
“Methylphenidate medications, when used as prescribed and in conjunction with behavioral therapy and lifestyle interventions, are one of the preferred first-line treatments for certain patients diagnosed with ADHD,” said Marcelo Bigal, MD, PhD, chief medical officer, Purdue Pharma, and general manager, Adlon Therapeutics. “We are pleased to receive FDA approval for Adhansia XR, a new option for appropriate patients with ADHD who may benefit from a treatment with efficacy demonstrated at one hour and 16 hours post-dose in adults, and we look forward to making it available later this year.”
The Full Prescribing Information for Adhansia XR contains a boxed warning for abuse and dependence. CNS stimulants, including Adhansia XR, other methylphenidate-containing products, and amphetamines have a high potential for abuse and dependence. Healthcare professionals should assess the risk of abuse prior to prescribing Adhansia XR and monitor for signs of abuse and dependence while patients are on therapy.
“Some of my patients with ADHD, especially those who are balancing school or work and participating in social or civic activities, require the ability to sustain attention throughout the day,” said Andrew J. Cutler, MD, chief medical officer, Meridien Research, and an investigator on Adhansia XR clinical studies. “The approval of Adhansia XR offers a methylphenidate treatment option with a longer duration of efficacy, which may be appropriate for these patients.”
Adhansia XR is not appropriate for all patients, and healthcare professionals should work with their patients to determine the most appropriate treatment option. Additionally, Adhansia XR is contraindicated in patients with a known hypersensitivity to methylphenidate or product components, as well as patients receiving concurrent treatment with a monoamine oxidase inhibitor (MAOI) or who have used an MAOI within the preceding 14 days.
The Full Prescribing Information for Adhansia XR, including Boxed Warning, is available at this link. Additionally, please see Important Safety Information for Adhansia XR below, including the Boxed Warning, Contraindications, Warnings and Precautions including the potential for abuse and dependence, serious cardiovascular events, blood pressure and heart rate increases, psychiatric adverse reactions, priapism, peripheral vasculopathy, long-term suppression of growth, allergic-type reactions, and Adverse Reactions.
“ADHD affects a significant number of adolescents and adults and, when not optimally treated, can negatively impact various aspects of their lives. A subset of these patients experience impairment throughout the day. While Adhansia XR is not appropriate for all patients, a methylphenidate medication available in a single daily dose that, in adults, demonstrated efficacy at one hour and at 16 hours post-dose, has the potential to address the needs of certain individuals with ADHD,” said Craig Landau, MD, president and CEO, Purdue Pharma. “We are committed to providing information on safe prescribing practices for this medication and initiatives to support the responsible use, storage, and disposal of all medications in this class."
The FDA approval of Adhansia XR was based on four clinical studies evaluating the efficacy and safety of Adhansia XR in patients who met DSM-5 criteria for ADHD. Eight hundred and eighty-three (883) patients were exposed to Adhansia XR during 1- to 4-week long, controlled treatment periods (434 adult patients and 449 pediatric patients [156 (6 to 12 years); 293 (12 to 17 years)] from two clinical studies in adults, one analog classroom trial over a 13-hour study day in pediatric patients ages 6 to 12 years, and one safety and efficacy study in pediatric patients ages 12 to 17 years). The safety data for adult patients are based on two randomized, double-blind, placebo-controlled studies in doses of 25 mg to 100 mg per day. The safety data for pediatric patients (6 to 17 years) are based on randomized, double-blind, placebo-controlled studies in doses of 25 mg to 85 mg per day.
A double-blind, randomized, placebo-controlled crossover AWE study evaluated Adhansia XR in adult patients with ADHD. Efficacy assessments were conducted at pre-dose and 1, 2, 5, 8, 11, 14, and 16 hours post-dose. The primary endpoint was the mean Permanent Measure of Performance Total scores (PERMP-T), averaged across all time points compared to placebo. PERMP-T, an objective, validated skill-adjusted math test, is the combined score obtained by adding PERMP-A (number of math problems attempted) and PERMP-C (number of math problems answered correctly).
While receiving Adhansia XR, adults achieved statistically significant improvement over placebo, achieving greater mean PERMP-T scores averaged across all time points on the AWE days (post-dose score of 281.3 vs. 254.5; difference of 26.80, 95% CI [15.19, 38.41]). The secondary efficacy endpoints were onset and duration of clinical effect, as assessed by the treatment difference in PERMP-T scores at post-dose time points. Adhansia XR demonstrated statistically significant improvement over placebo at 1, 2, 5, 8, 11, and 16 hours post-dose, but not at hour 14 post-dose.
In this study, 10% of Adhansia XR-treated patients discontinued due to adverse reactions compared to 0% of placebo-treated patients. The following adverse reactions led to discontinuation at a frequency of 2% of Adhansia XR-treated patients: nausea, bronchitis, viral gastroenteritis, viral infection, increased blood pressure, and hypomania.
Sudden death, stroke and myocardial infarction have occurred in patients treated with CNS stimulants at recommended doses. Additional information about serious cardiovascular risks can be found in the Important Safety Information section below.
Adhansia XR will be available in six capsule strengths (25, 35, 45, 55, 70, and 85 mg), allowing for flexible dosing. The recommended starting dose of Adhansia XR for patients six years or older is 25 mg once daily. Healthcare professionals should titrate the dose in increments of 10 mg to 15 mg at intervals of no less than five days. Adhansia XR should be taken orally once daily in the morning, with or without food. Capsules may be taken whole or, for patients who have difficulty swallowing, capsules may be opened and the entire contents sprinkled onto a tablespoon of applesauce or yogurt. The entire mixture should be consumed without crushing or chewing, immediately or within 10 minutes. If the mixture is not consumed within 10 minutes after mixing, it should be discarded and not stored. The dose of a single capsule should not be divided and patients should not take anything less than one capsule per day. In the event of a missed dose, patients should not take their medication later in the day.
Prior to initiating treatment with Adhansia XR, healthcare professionals should also assess for the presence of cardiac disease (i.e., perform a careful history, family history of sudden death or ventricular arrhythmia, and physical exam). Healthcare professionals should assess the risk of abuse prior to prescribing Adhansia XR and monitor for signs of abuse and dependence while patients are on therapy. After prescribing and while patients are on therapy, healthcare professionals should maintain careful prescription records, educate patients and their families about abuse and proper storage and disposal of CNS stimulants, and periodically re-evaluate the need for Adhansia XR use.
Dosages above 85 mg daily in adults and 70 mg and above daily in pediatric patients are associated with disproportionate increases in the incidence of certain adverse reactions. If paradoxical aggravation of symptoms or other adverse reactions occur, healthcare professionals should reduce the dosage, or, if necessary, discontinue treatment with Adhansia XR. Treatment with Adhansia XR should also be periodically discontinued to assess the patient's condition. If improvement is not observed in a patient after appropriate dosage adjustment over a one-month period, healthcare providers should discontinue treatment with Adhansia XR.1 Healthcare professionals should refer to the Full Prescribing Information for additional Dosage and Administration information.
Prescription stimulants, which include methylphenidate, the active ingredient in Adhansia XR, are federally controlled substances (CII) and have a high potential for abuse and dependence.1,2 The selling or giving away of methylphenidate medications may harm others or lead to death, and is against the law. It is important for healthcare professionals to ask patients if they or a family member have ever misused prescription medicines or abused alcohol or street drugs. Patients should be counseled that they should not give Adhansia XR to anyone else, and to keep methylphenidate medications in a safe place, such as a locked cabinet, to help prevent accidental exposure, diversion, and abuse. They should also be advised to dispose of remaining, unused, or expired Adhansia XR by a medicine take-back program at authorized collection sites such as pharmacies or law enforcement locations, if available. If no take-back program or authorized collector is available, patients should mix Adhansia XR with an undesirable, nontoxic substance to make it less appealing to children and pets, place the mixture in a container such as a sealed plastic bag, and discard of it in the household trash.1 Patients should be encouraged to read the Medication Guide that accompanies their stimulant prescription, which contains the most important FDA-approved information that a patient should know about the medication
REf: https://en.wikipedia.org/wiki/Methylphenidate