Tuesday, April 1, 2014
Tuesday, April 2, 2019
Some drug combinations may be more effective than others for schizophrenic patients
Monday, November 9, 2015
Vraylar (cariprazine) capsules now approved by FDA to treat schizophrenia, bipolar disorder in adults

Monday, May 22, 2017
Drugs designed to target nervous system could control inflammation in the gut, study shows
"We are talking about an existing set of drugs and drug targets that could open up the spectrum of potential therapeutic applications by targeting pathways that fine-tune the inflammatory response," said Alejandro Aballay, Ph.D., a professor of molecular genetics and microbiology at Duke School of Medicine.
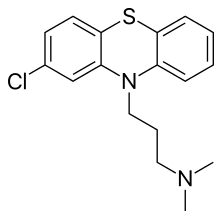
"Worms have evolved mechanisms to deal with colonizing bacteria," Aballay said. "That is true for us as well. Humans have trillions of microorganisms in our guts, and we have to be careful when activating antimicrobial defenses so that we mainly target potentially harmful microbes, without damaging our good bacteria -- or even our own cells -- in the process."
Friday, March 4, 2016
Add-on lamotrigine enhances bipolar depression treatment

Tuesday, November 17, 2020
Kratom Seems Safe for Pain, Anxiety, Opioid Withdrawal

https://www.sciencedirect.com/science/article/abs/pii/S0376871620300144
https://en.wikipedia.org/wiki/Mitragyna_speciosa
Thursday, October 16, 2014
Sunday, February 28, 2010
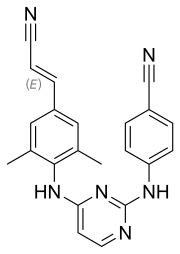
Serotonin-Specific Reuptake Inhibitor (SSRIs) as antiinflammatory agents?
Researchers observed reduced inflammation, reduced cartilage and bone erosion, and a preservation of the joint structure in the mice treated with a higher dose of fluoxetine. Citalopram was not as effective as fluoxetine at inhibiting disease progression in this model.
Monday, November 27, 2017
FDA Approves Abilify MyCite (aripiprazole) Pill with Sensor to Digitally Track if Patients Have Ingested Their Medication

The U.S. Food and Drug Administration today approved the first drug in the U.S. with a digital ingestion tracking system. Abilify MyCite (aripiprazole tablets with sensor) has an ingestible sensor embedded in the pill that records that the medication was taken. The product is approved for the treatment of schizophrenia, acute treatment of manic and mixed episodes associated with bipolar I disorder and for use as an add-on treatment for depression in adults.
Wednesday, February 13, 2013
Top-line results from Vanda's tasimelteon Phase IIb/III study on major depressive disorder
A year-long (2011-2012) study at Harvard is testing the use of tasimelteon in blind subjects with non-24-hour sleep-wake disorder.
"These results are disappointing, as there is still a significant unmet medical need for patients with Major Depression," said Mihael H. Polymeropoulos , M.D., President and CEO of Vanda. "Tasimelteon's application in the treatment of blind individuals with Non-24 remains our top priority as we pursue our planned NDA submission this year."
Vanda has recently reported positive results in two phase III clinical studies of tasimelteon in Non-24-Hour Disorder (Non-24) and plans to submit a New Drug Application to the U.S. Food and Drug Administration in mid-2013......
Monday, June 28, 2021
Drug commonly used as antidepressant helps fight cancer in mice
A new study by UCLA researchers suggests that those drugs, commonly known as MAOIs, might have another health benefit: helping the immune system attack cancer. Their findings are reported in two papers, which are published in the journals Science Immunology and Nature Communications.
"MAOIs had not been linked to the immune system's response to cancer before," said Lili Yang, senior author of the study and a member of the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA. "What's especially exciting is that this is a very well-studied and safe class of drug, so repurposing it for cancer isn't as challenging as developing a completely new drug would be."
Recent advances in understanding how the human immune system naturally seeks out and destroys cancer cells, as well as how tumors try to evade that response, has led to new cancer immunotherapies—drugs that boost the immune system's activity to try to fight cancer.
In an effort to develop new cancer immunotherapies, Yang and her colleagues compared immune cells from melanoma tumors in mice to immune cells from cancer-free animals. Immune cells that had infiltrated tumors had much higher activity of a gene called monoamine oxidase A, or MAOA. MAOA's corresponding protein, called MAO-A, controls levels of serotonin and is targeted by MAOI drugs.
"For a long time, people have theorized about the cross-talk between the nervous system and the immune system and the similarities between the two," said Yang, who is also a UCLA associate professor of microbiology, immunology and molecular genetics and a member of the UCLA Jonsson Comprehensive Cancer Center. "So it was exciting to find that MAOA was so active in these tumor-infiltrating immune cells."
Next, the researchers studied mice that didn't produce MAO-A protein in immune cells. The scientists found that those mice were better at controlling the growth of melanoma and colon tumors. They also found that normal mice became more capable of fighting those cancers when treated with MAOIs.
Digging in to the effects of MAO-A on the immune system, the researchers discovered that T cells—the immune cells that target cancer cells for destruction—produce MAO-A when they recognize tumors, which diminishes their ability to fight cancer.
That discovery places MAO-A among a growing list of molecules known as immune checkpoints, which are molecules produced as part of a normal immune response to prevent T cells from overreacting or attacking healthy tissue in the body. Cancer has been known to exploit the activity of other previously identified immune checkpoints to evade attack by the immune system.
In the Science Immunology paper, the scientists report that MAOIs help block the function of MAO-A, which helps T cells overcome the immune checkpoint and more effectively fight the cancer.
But the drugs also have a second role in the immune system, Yang found. Rogue immune cells known as tumor-associated macrophages often help tumors evade the immune system by preventing anti-tumor cells including T cells from mounting an effective attack. High levels of those immunosuppressive tumor-associated macrophages in a tumor have been associated with poorer prognoses for people with some types of cancer.
But the researchers discovered that MAOIs block immunosuppressive tumor-associated macrophages, effectively breaking down one line of defense that tumors have against the human immune system. That finding is reported in the Nature Communications paper.
"It turns out that MAOIs seem to both directly help T cells do their job, and stop tumor-associated macrophages from putting the brakes on T cells," Yang said.
Combining MAOIs with existing immunotherapies
Yang said she suspects that MAOIs may work well in concert with a type of cancer immunotherapies called immune checkpoint blockade therapies, most of which work by targeting immune checkpoint molecules on the surface of immune cells. That's because MAOIs work on MAO-A proteins, which are inside cells and function differently from other known immune checkpoint molecules.
Studies in mice showed that any of three existing MAOIs—phenelzine, clorgyline or mocolobemide—either on their own or in combination with a form of immune checkpoint blockade therapy known as PD-1 blockers, could stop or slow the growth of colon cancer and melanoma.
Although they haven't tested the drugs in humans, the researchers analyzed clinical data from people with melanoma, colon, lung, cervical and pancreatic cancer; they found that people with higher levels of MAOA gene expression in their tumors had, on average, shorter survival times. That suggests that targeting MAOA with MAOIs could potentially help treat a broad range of cancers.
Yang and her collaborators are already planning additional studies to test the effectiveness of MAOIs in boosting human immune cells' response to various cancers.
Yang said MAOIs could potentially act on both the brain and immune cells in patients with cancer, who are up to four times as likely as the general population to experience depression.
"We suspect that repurposing MAOIs for cancer immunotherapy may provide patients with dual antidepressant and antitumor benefits," she said.
The experimental combination therapy in the study was used in preclinical tests only and has not been studied in humans or approved by the Food and Drug Administration as safe and effective for use in humans. The newly identified therapeutic strategy is covered by a patent application filed by the UCLA Technology Development Group on behalf of the Regents of the University of California, with Yang, Xi Wang and Yu-Chen Wang as co-inventors.
Tuesday, March 23, 2010
Clinical Data completes NDA submission for vilazodone.......
This is a major milestone in the development of vilazodone and, if approved, its dual mechanism of action and safety profile will offer a new alternative for patients suffering from depression,” said Carol R. Reed, M.D..more...
Wednesday, November 22, 2017
FDA Approves Juluca, First Two-Drug Regimen for HIV Patients
 rilpivirine
rilpivirine  Dolutegravir
Dolutegravir“Limiting the number of drugs in any HIV treatment regimen can help reduce toxicity for patients,” said Debra Birnkrant, MD, director of the Division of Antiviral Products in the FDA’s Center for Drug Evaluation and Research.
Wednesday, August 4, 2010
Scientists develop obesity drug without neurological side effects....
As per the claim by the researchers, this drug did not cause weight loss or neurological side effects, which rimonabant does, but did have effects on levels of glucose and fats in the blood that should reduce the risk of the serious health consequences of obesity.
The authors therefore hope that this approach of targeting only peripheral CB1R can be translated into the clinic to reduce health risks in obese patients..
Tuesday, June 11, 2019
Veggies, Fruits and Grains Keep Your Heart Pumping
- Convenience, which was heavy on meats, pasta, Mexican food, pizza and fast food.
- Plant-based, which included vegetables, fruits, beans and fish.
- Sweets and fats, which was heavy on desserts, bread, sweet breakfast foods, chocolate and other sugars.
- Southern, which was heavy on fried foods, processed meats, eggs, added fats, and sugar-sweetened drinks.
- Alcohol and salads, which was heavy on wine, liquor, beer, leafy greens and salad dressing.



