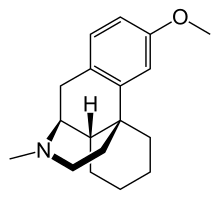
dextromethorphan

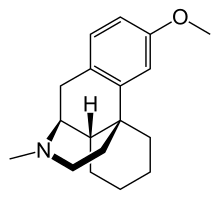
Bupropion
In continuation of my updates on dextromethorphan and Bupropion,
Axsome Therapeutics, Inc. , a biopharmaceutical company
developing and delivering novel therapies for the management of central
nervous system (CNS) disorders, announced the U.S. Food and
Drug Administration (FDA) approval of Auvelity (dextromethorphan HBr -bupropion HCl) extended-release tablets for the treatment of major depressive disorder (MDD) in adults.1
Auvelity is the first and only rapid-acting oral medicine approved for
the treatment of MDD with labeling of statistically significant
antidepressant efficacy compared to placebo starting at one week. The rapid antidepressant effects of Auvelity were sustained at all subsequent timepoints. Auvelity is the first and only oral N-methyl D-aspartate (NMDA) receptor antagonist approved for the treatment of MDD. Axsome anticipates Auvelity to be commercially available in the U.S. in the fourth quarter of 2022.
Maurizio Fava, MD, Psychiatrist-In-Chief, Department of Psychiatry,
Massachusetts General Hospital, Executive Director, Clinical Trials
Network & Institute, Associate Dean for Clinical & Translational
Research, and Slater Family Professor of Psychiatry, Harvard Medical
School said, “The approval of Auvelity represents a milestone in
depression treatment based on its novel oral NMDA antagonist mechanism,
its rapid antidepressant efficacy demonstrated in controlled trials, and
a relatively favorable safety profile. Auvelity, which was granted
Breakthrough Therapy designation by the FDA, represents the first new
oral non-monoamine-based mechanism of action approved to treat major
depressive disorder in over sixty years. Nearly two thirds of patients
treated with currently available antidepressants do not adequately
respond, and those that do may not achieve clinically meaningful
responses for up to six to eight weeks. Given the debilitating nature of
depression, the efficacy of Auvelity observed at one week and sustained
thereafter may have a significant impact on the current treatment
paradigm for this condition.”
Michael Pollock, Chief Executive Officer of the Depression and
Bipolar Support Alliance (DBSA), a leading national patient advocacy
organization focusing on depression and bipolar disorder said, “The
mental health crisis in the United States is one of the most pressing
health issues facing our country today. Over 20 million American adults
experienced major depressive disorder each year prior to the COVID-19
pandemic. These numbers increased dramatically during the pandemic with
approximately thirty percent of adults in the U.S. or more than 80
million Americans experiencing elevated symptoms of depression. The need
for new treatment options, particularly those with new mechanisms of
action, could not be clearer and more urgent for those living with, or
impacted by, major depressive disorder.”
Dan V. Iosifescu, MD, Professor of Psychiatry at the New York
University School of Medicine, and Director of the Clinical Research
Division at the Nathan Kline Institute for Psychiatric Research said,
“Major depressive disorder is disabling and potentially
life-threatening, causes profound distress for patients and their
families, and leads to substantial healthcare resource utilization.
Auvelity’s oral NMDA receptor antagonist and sigma-1 receptor agonist
activity, which targets glutamatergic neurotransmission, provides
clinicians a long sought after new mechanistic approach which may
benefit the millions of patients living with this serious condition. In
clinical trials, Auvelity has demonstrated rapid and statistically
significant improvement in depressive symptoms as early as Week 1, and
increased rates of remission at Week 2 compared with placebo. This early
benefit with Auvelity was maintained and increased with continued
treatment, and was accompanied by a favorable safety and tolerability
profile.”
Auvelity was studied in a comprehensive clinical program which
included more than 1,100 patients with depression. The efficacy of
Auvelity in the treatment of MDD was demonstrated in the GEMINI
placebo-controlled study, and confirmatory evidence which included the
ASCEND study comparing Auvelity to bupropion sustained-release tablets.
In the GEMENI study, Auvelity was statistically significantly superior
to placebo in improvement of depressive symptoms as measured by the
change in the Montgomery-Åsberg Depression Rating Scale (MADRS) total
score at Week 6, the study’s primary endpoint. To evaluate speed of
onset of action, the change in MADRS total score from baseline to Week 1
and from baseline to Week 2 were pre-specified secondary efficacy
endpoints. The difference between Auvelity and placebo in change from
baseline in MADRS total score was statistically significant at Week 1
and at Week 2.1 In the ASCEND study, Auvelity was
statistically significantly superior to bupropion sustained-release
tablets 105 mg twice daily on the primary outcome measure.5
The primary outcome measure of the ASCEND study was calculated by
assessing the change from baseline in MADRS total scores from Week 1 to
Week 6 and then taking the average of those scores.1 In the
placebo-controlled clinical study, the most common (incidence ≥5% for
Auvelity and more than twice as frequently as placebo) adverse reactions
were dizziness, headache, diarrhea, somnolence, dry mouth, sexual
dysfunction, and hyperhidrosis.1
The FDA granted Breakthrough Therapy designation for Auvelity for the
treatment of MDD in March 2019. This designation is granted to
candidate drugs that show potential for benefit above that of available
therapies based on preliminary clinical data, and it provides the
sponsor with added focus from and greater interactions with FDA staff
during the development of the candidate drug.6 The Auvelity
New Drug Application (NDA) was evaluated by the FDA under Priority
Review, which is granted by the FDA to applications for medicines that,
if approved, would provide significant improvements in the effectiveness
or safety of the treatment, diagnosis, or prevention of serious
conditions when compared to standard applications.
https://en.wikipedia.org/wiki/Bupropion
https://en.wikipedia.org/wiki/Dextromethorphan