Vertex Pharmaceuticals Incorporated (Nasdaq: VRTX) announced U.S. Food and Drug Administration (FDA) approval of Journavx (suzetrigine), an oral, non-opioid, highly selective NaV1.8 pain signal inhibitor for the treatment of adults with moderate-to-severe acute pain. Journavx is an effective, well-tolerated medicine without evidence of addictive potential indicated for use across all types of moderate-to-severe acute pain.
“Today’s approval is a historic milestone for the 80 million people in America who are prescribed a medicine for moderate-to-severe acute pain each year,” said Reshma Kewalramani, M.D., Chief Executive Officer and President of Vertex. “With the approval of Journavx, a non-opioid, pain signal inhibitor and the first new class of pain medicine approved in more than 20 years, we have the opportunity to change the paradigm of acute pain management and establish a new standard of care.”
“This is an incredible day for patients and physicians alike who now have an approved non-opioid treatment that delivers effective acute pain relief and a favorable safety profile without addictive potential,” said Jessica Oswald, M.D., M.P.H., Associate Physician in Emergency Medicine and Pain Medicine in San Diego and Vertex Acute Pain Steering Committee Member. “I believe Journavx could redefine the management of pain and become a foundational treatment option for people with all types of moderate-to-severe acute pain, where options aside from opioids have been so desperately needed.”
As part of Vertex’s ongoing commitment to patients, the company has established patient support programs to help ensure that qualified patients can access Journavx. For more information visit Journavx.com.
About Acute Pain
Acute pain is a serious and potentially disabling condition often caused by surgery, accident or injury. Over 80 million Americans are prescribed medicine to treat their moderate-to-severe acute pain every year. Of these, about 40 million are prescribed an opioid. Nearly 10% of acute pain patients treated initially with an opioid will go on to have prolonged opioid use, and about 85,000 patients will develop opioid use disorder annually. Poorly controlled acute pain can lead to reduced quality of life, development of chronic pain, and increased burden on the health care system and society.
About Journavx (suzetrigine)
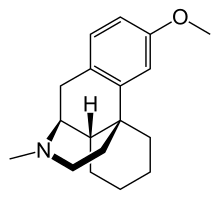
Journavx (suzetrigine) is a first-in-class, oral, non-opioid, highly selective pain signal inhibitor that is selective for NaV1.8 relative to other NaV channels. NaV1.8 is a voltage-gated sodium channel that is selectively expressed in peripheral pain-sensing neurons (nociceptors), where its role is to transmit pain signals (action potentials). Because Journavx blocks pain signals only found in the periphery, not in the brain, Journavx provides effective relief of pain without the limitations of currently available therapies, including the addictive potential of opioids.
The U.S. Food and Drug Administration approved twice-daily Journavx for the treatment of adults with moderate-to-severe acute pain. Vertex has established a wholesale acquisition cost for Journavx in the United States of $15.50 per 50mg pill.
Vertex is also evaluating suzetrigine in peripheral neuropathic pain (PNP). The company’s Phase 3 pivotal program for suzetrigine in patients with painful diabetic peripheral neuropathy is ongoing, and Vertex plans to advance its pivotal program evaluating suzetrigine in patients with painful lumbosacral radiculopathy pending discussions with regulators.
INDICATION and IMPORTANT SAFETY INFORMATION
INDICATION AND USAGE
Journavx is a prescription medicine used to treat adults with moderate-to-severe short term (acute) pain.
It is not known if Journavx is safe and effective in children.
IMPORTANT SAFETY INFORMATION
Patients should not take Journavx if they take certain medicines that are strong inhibitors of an enzyme called CYP3A. Patients should ask their healthcare providers if they are not sure.
Before taking Journavx, patients should tell their healthcare provider about all of their medical conditions, including if they: have liver problems. People with liver problems may have an increased risk of getting side effects from taking Journavx; are pregnant or plan to become pregnant as it is not known if Journavx will harm an unborn baby. Patients and their healthcare providers should decide if they will take Journavx while they are pregnant, are breastfeeding, or are planning to breastfeed, as it is not known if Journavx passes into breast milk. Patients and their healthcare providers should decide if they will take Journavx while they are breastfeeding.
Patients should tell their healthcare provider about all the medicines they take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Taking Journavx with certain other medicines may affect the way Journavx and the other medicines work and may increase patients’ risk of side effects. Patients should ask their healthcare provider or pharmacist for a list of these medicines if they are not sure.
Patients should especially tell their healthcare provider if they take hormonal birth control medicine (contraceptives) containing progestins other than levonorgestrel or norethindrone. If they take one of these contraceptives (progestins other than levonorgestrel or norethindrone), they may not work as well during treatment with Journavx. Patients should also use nonhormonal contraceptives such as condoms or use other forms of hormonal birth control during treatment with Journavx and for 28 days after they stop taking Journavx. Medicines that are substrates of the CYP3A enzyme may become less effective during treatment with Journavx. Their healthcare provider may need to adjust the dose of patients’ medicine when starting or stopping Journavx. Patients should know the medicines they take and keep a list of them to show their healthcare provider and pharmacist when they get a new medicine. Patients should not take food or drink containing grapefruit while taking Journavx.
Journavx can cause side effects: The most common side effects for patients treated with Journavx include itching, muscle spasms, increased blood level of creatine phosphokinase, and rash. Journavx may temporarily reduce the chance of females becoming pregnant while on treatment. Patients should talk to their healthcare provider if they have concerns about becoming pregnant. If patients are using contraceptives, continue to use contraceptives during treatment with Journavx. Patients should tell their healthcare provider if they have any side effect that bothers them or that does not go away. These are not all of the possible side effects of Journavx. Patients should call their healthcare provider for medical advice about side effects. Patients may report side effects to the FDA at 1-800-FDA-1088.
About Vertex
Vertex is a global biotechnology company that invests in scientific innovation to create transformative medicines for people with serious diseases. The company has approved medicines that treat the underlying causes of multiple serious diseases and conditions — cystic fibrosis, sickle cell disease, transfusion-dependent beta thalassemia and acute pain — and continues to advance clinical and research programs in these areas. Vertex also has a robust clinical pipeline of investigational therapies across a range of modalities in other serious diseases where it has deep insight into causal human biology, including neuropathic pain, APOL1-mediated kidney disease, IgA nephropathy, primary membranous nephropathy, autosomal dominant polycystic kidney disease, type 1 diabetes and myotonic dystrophy type 1.