Wednesday, March 31, 2021
Statin use alone or with metformin may increase survival in high-risk prostate cancer patients
Thursday, March 14, 2019
Statins Help the Heart, No Matter What Your Age
Cholesterol-lowering statins are already known to help cut heart risks for seniors and the middle-aged. Now, research confirms the meds can also help people aged 75 and older.
"Statin therapy has been shown to prevent cardiovascular disease in a wide range of people, but there has been uncertainty about its efficacy and safety among older people," said lead investigator Anthony Keech. He's a professor of medicine, cardiology and epidemiology at the University of Sydney in Australia.
"Our study summarized all the available evidence from major trials to help clarify this issue. We found that there were significant reductions in major vascular events in each of the six age groups considered, including patients [who were] aged over 75 at the start of treatment," Keech said in an Oxford news release.
"Statin therapy appears to be just as effective in people aged over 75 years as it is in younger people," study co-investigator Jordan Fulcher said in the news release. Fulcher is a cardiovascular research fellow at the University of Sydney.
"We have definitive evidence that statins benefit older people who have suffered a heart attack or stroke. Fewer healthy older people were represented in these trials, so more information in this group of people would help confirm the same benefits that we see in our overall trials population," he said.
"Since the risk of heart attack and stroke increases with age, the potential benefits are likely to be even greater for older people," he said.
"Therefore, there is a need to ensure that patients at risk of cardiovascular disease due to their age are offered statin therapy where there is good reason to believe that it will be beneficial," Baigent said.
Monday, October 24, 2016
Statins may shield unborn babies from mother's stress, study suggests
Thursday, December 11, 2014
Cholesterol-fighting statins inhibit uterine fibroid tumors that account for 50% of hysterectomies...
Monday, November 16, 2009
Statins as anticancer and anti diabetic agents ?
Statins lower cholesterol by blocking certain enzymes involved in our metabolism. However, they have also been shown to affect other important lipids in the body, such as the lipids that help proteins to attach to the cell membrane (known as lipid modification). Because many of the proteins that are lipid-modified cause cancer, there are now hopes that it will be possible to use statins in the treatment of cancer.
Studies show that statins can have a dramatic inhibitory effect on growth and development. As the researchers managed to identify the enzyme involved, they can also explain how the effect arises at molecular level. Not least that they can prevent the growth of cancer cells caused by lipid-modified proteins, but also that they can be effective in the treatment of diabetes and neurological disorders such as Parkinson's. In one of my earlier blog, I have mentioned about the simvastin (Simvastatin prevents progression of Parkinson's Disease ?).
So in the days to come statins may be useful as anticancer, anti diabetic and even to treat Parkinsons disaese....
Source : http://www.science.gu.se/english/News/News_detail/Cholesterol-lowering_medicines_may_be_effective_against_cancer.cid898016
Friday, January 29, 2021
Statins May Protect Heart From Chemo for Early Breast Cancer
For women with early breast cancer treated with anthracyclines, statin exposure is associated with a lower risk for hospital presentation for heart failure, according to a study published online Jan. 6 in the Journal of the American Heart Association.
Husam Abdel-Qadir, M.D., Ph.D., from the Women's College Hospital in Toronto, and colleagues conducted a retrospective cohort study involving women aged 66 years and older without prior heart failure who received anthracyclines or trastuzumab for newly diagnosed early breast cancer. Using propensity scores, statin-exposed and unexposed women were matched in a 1:1 ratio. Data were included for 666 statin-discordant pairs of anthracycline-treated women and 390 pairs of trastuzumab-treated women.
The researchers found that the five-year cumulative incidence of heart failure hospital presentations after anthracyclines was 1.2 percent (95 percent confidence interval [CI], 0.5 to 2.6 percent) and 2.9 percent (95 percent CI, 1.7 to 4.6 percent) in statin-exposed and unexposed women, respectively (P = 0.01). In the anthracycline cohort, the cause-specific hazard ratio associated with statins was 0.45 (95 percent CI, 0.24 to 0.85; P = 0.01). The five-year cumulative incidence of heart failure hospital presentations after trastuzumab was 2.7 percent (95 percent CI, 1.2 to 5.2 percent) and 3.7 percent (95 percent CI, 2.0 to 6.2 percent) in statin-exposed and unexposed women, respectively (P = 0.09), with a cause-specific hazard ratio associated with statins of 0.46 (95 percent CI, 0.20 to 1.07; P = 0.07).
"This study does not conclusively prove statins are protective," Abdel-Qadir said in a statement. "However, this study builds on the body of evidence suggesting that they may have benefits."
Saturday, July 6, 2019
Statin Use Associated With Higher Incidence of Diabetes
"As lifestyle programs like the Diabetes Prevention Program are promoted in primary care settings, we hope physicians will integrate and insurers support healthy lifestyle strategies as part of the optimal management of individuals at risk for both new-onset diabetes and cardiovascular disease," the authors write.
Friday, April 11, 2014
Statins could ease coughing in lung disease patients, study finds -- ScienceDaily
Monday, March 15, 2010
Eprotirome a promising addition to statin therapy ?
Interestingly, the researchers caution that the results don't suggest that eprotirome will or should replace statins, which are the current gold standard for treating high LDL cholesterol.
Friday, August 14, 2015
Cholesterol-lowering statin drugs could delay prostate cancer growth in patients receiving ADT
Sunday, January 6, 2013
Common cholesterol-lowering drug may help protect against cerebral malaria
"The molecular mechanisms that give rise to cerebral malaria and subsequent cognitive dysfunction are not yet known," says Zimmerman. "However, the fact that statin treatment decreases both injurious blood vessel inflammation and cognitive dysfunction suggests that a combination of vascular and inflammatory triggers leads to cerebral pathology and intellectual deficits."Ref : http://www.plospathogens.org/article/info%3Adoi%2F10.1371%2Fjournal.ppat.1003099
Common cholesterol-lowering drug may help protect against cerebral malaria
Friday, June 8, 2012
Experimental cholesterol drug, REGN727 (PCSK9 inhibitor) results called ‘game changing
“Wars for PCSK9 are far bigger than the statin wars,” said Dr. Evan A Stein, lead author of the study and researcher at the Metabolic and Atherosclerosis Research Center in Cincinnati, Ohio. “This is a hot research area and everybody is so close together.”
Thursday, September 14, 2017
Fenofibrate drug may reduce risk of cardiovascular events in patients with type 2 diabetes

Friday, June 17, 2016
Evolocumab could be more effective than ezetimibe in lowering cholesterol in statin-intolerant patients

- In Phase A, patients were assigned to two groups. Each group was treated for 10 weeks with atorvastatin or placebo in a blinded fashion, then crossed over to the alternate therapy for another 10 weeks. Patients were asked to report any muscle pain or weakness.
- Patients who reported intolerable muscle symptoms on atorvastatin, but not placebo, moved to Phase B. In this 24-week phase, patients with confirmed statin intolerance were administered two alternative non-statin therapies, ezetimibe vs. evolocumab.
- The research is being presented at the American College of Cardiology's 65th Annual Scientific Session and simultaneously published online in the Journal of the American Medical Association."Statin intolerance has been a very challenging clinical problem," said Steven Nissen, M.D., chairman of Cardiovascular Medicine at Cleveland Clinic. "The study showed that PCSK9 inhibitors can significantly lower cholesterol in patients with documented statin intolerance, providing an effective treatment for these difficult to manage patients."The GAUSS-3 trial enrolled 511 patients with very high levels of LDL cholesterol - averaging more than 210 mg/dL ¬¬- and with a history of muscle-related statin intolerance. More than 80% of participants had previously reported intolerance to three or more statins. The study showed that 42.6 percent of these patients reported muscle pain or weakness on atorvastatin, but not placebo, and 26.5 percent on the placebo, but not atorvastatin.
Friday, April 14, 2017
New research shows how cholesterol medicine has beneficial effect on immune defence system
Saturday, December 5, 2009
Thursday, November 5, 2009
Lovastatin-synthesizing enzyme successfully reconstituted...

Dield-Alder catalysed cyclisation : In vitro formation of a triketide lactone using a genetically-modified protein derived from 6-deoxyerythronolide B synthase has been demonstrated. The stereochemistry of the molecule supports the intriguing idea that an enzyme-catalyzed Diels-Alder reaction may occur during assembly of the polyketide chain. It thus appears that biological Diels-Alder reactions may be triggered by generation of reactive triene systems on an enzyme surface.
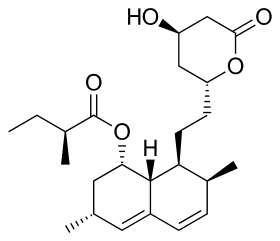
Biosynthesis using broadly specific acyltransferase : It has been found that a dedicated acyltransferase, LovD, is encoded in the lovastatin biosynthetic pathway. LovD has a broad substrate specificity towards the acyl carrier, the acyl substrate and the decalin acyl acceptor. It efficiently catalyzes the acyl transfer from coenzyme A thoesters or N-acetylcysteamine (SNAC) thioesters to monacolin J. The biosynthesis of lovastatin is coordinated by two iterative type I polyketide syntheses and numerous accessory enzymes. Nonketide, the intermediate biosynthetic precursor of lovastatin, is assembled by the upstream megasynthase LovB (also known as lovastatin nonaketide synthase), enoylreductase LovC, and CYP450 oxygenases.
Recently more interesting out come from a group of UCLA researchers is that, for the first time thy have successfully reconstituted in the laboratory the enzyme responsible for producing the blockbuster cholesterol-lowering drug lovastatin. As per the claim by the researchers, the lovastatin-synthesizing enzyme is one of the most interesting but least understood of the polyketide synthases, which are found in filamentous fungi and which play a crucial role in the synthesis of "small molecule natural products" — pharmacologically or biologically potent compounds produced by living organisms, many of which are the active ingredients in pharmaceuticals.
This finding is of great significance because commonly used antibiotics, such as tetracycline, are produced by polyketide synthases. Polyketides represent a class of 7,000 known structures, of which more than 20 are commercial drugs, including the immunosuppressant rapamycin, the antibiotic erythromycin and the anticancer drug doxorubicin. In their study studied the enzyme that makes a small-molecule precursor to lovastatin. The real difference about this enzyme, is its extraoridnarily large size in comparison to all other enzymes so for studied. As per the claim by the lead researcher Dr. Yi Tang, "It's one of the largest enzymes ever to be reconstituted in a test tube. It is 10 times the size of most enzymes people study & the enzyme has seven active sites and catalyzes more than 40 different reactions that eventually result in an important precursor to lovastatin. Hope with this remarkable achievement, one can prepare many natural products in the lab in the days to come.
Ref : http://www.newsroom.ucla.edu/portal/ucla/ucla-engineering-researchers-have-111812.aspx
Friday, November 1, 2013
New Cholesterol-Lowering Drug, ALN-PCS Shows Early Promise
"Cardiovascular disease remains the leading cause of death of men and women globally and reduction of LDL cholesterol with statin medications has been demonstrated to substantially reduce the risk of first or recurrent cardiovascular events," said Dr. Gregg Fonarow, a professor of cardiology at the University of California, Los Angeles.
Wednesday, January 13, 2021
AHA: Adding Omega-3 Fatty Acids Does Not Cut High CV Risk
In continuation of my update on omega-3 fatty acids
A carboxylic acid formulation of eicosapentaenoic acid and docosahexaenoic acid (omega-3 CA) does not improve outcomes among statin-treated patients at high cardiovascular risk, according to a study published online Nov. 15 in the Journal of the American Medical Association to coincide with the American Heart Association Scientific Sessions 2020, held virtually from Nov. 13 to 17.
Stephen J. Nicholls, M.B.B.S., Ph.D., from Monash University in Melbourne, Australia, and colleagues conducted a double-blind trial comparing omega-3 CA to corn oil in 13,078 statin-treated patients with high cardiovascular risk, hypertriglyceridemia, and low high-density lipoprotein cholesterol from 675 academic and community hospitals in 22 countries. Participants were randomly assigned in a 1:1 ratio to either 4 g/day omega-3 CA or corn oil (6,539 to each) in addition to usual background therapies, including statins.
"These findings do not support use of this omega-3 fatty acid formulation to reduce major adverse cardiovascular events in high-risk patients," the authors write.
Several authors disclosed financial ties to pharmaceutical companies, including AstraZeneca, which funded the study.
Saturday, November 14, 2009
Simvastatin prevents progression of Parkinson's Disease ?

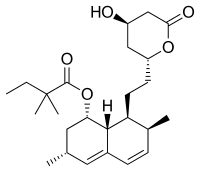
Simvastatin, (marketed under the names Zocor, Simlup, Simcard, Simvacor) is a hypolipidemic drug belonging to the class of pharmaceuticals called "statins". It is used to control hypercholesterolemia and to prevent cardiovascular disease. Simvastatin is a synthetic derivate of a fermentation product of Aspergillus terreus. When I was working with Bangalore based company, the sister company was working on it and now its marketing too.
Recently researchers from the Rush University, have found an interesting fact that Simvastin, may prevent Parkinson's disease from progressing further. The authors have shown that the activity of one protein called p21Ras is increased very early in the midbrain of mice with Parkinson's pathology. Simvastatin enters into the brain and blocks the activity of the p21Ras protein and other associated toxic molecules, and goes on to protect the neurons, normalize neurotransmitter levels, and improves the motor functions in the mice with Parkinson's.
If the researchers are able to replicate these results in Parkinson's patients in the clinical setting, it would be a remarkable advance in the treatment of this devastating neurodegenerative disease. Hope some relief to the sufferers of Parkinson disease....
Ref : http://www.rush.edu/webapps/MEDREL/servlet/NewsRelease?id=1304


