"The magnitude of this reduction in LDL-C and the fact that some patients reached or approached the LDL-C therapeutic goals is truly remarkable for this high risk population that historically doesn't respond to lipid-lowering drugs," said the study's lead author, Marina Cuchel, MD, PhD, research assistant professor of Medicine at Penn. "A reduction in LDL-C of this magnitude is certainly expected to favorably alter the clinical course of this devastating disease."
Friday, November 9, 2012
New medication lomitapide, shows promise as lipid-lowering therapy for rare cholesterol disorder
Thursday, April 9, 2020
Aspirin May No Longer Have Effect in Primary CVD Prevention
"In a modern era characterized by widespread statin use and population-wide cancer screening, aspirin no longer reduces the absolute risk of cancer death or myocardial infarction when given as primary prevention," the authors write.
Wednesday, September 20, 2017
Two anticlotting medicines better at reducing bleeding risk than triple therapy
 rivaroxaban
rivaroxaban 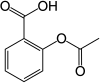 Aspirin
AspirinFriday, November 20, 2009
Positive results from mipomersen- a new hope for FH sufferers...
Familial hypercholesterolemia (also spelled familial hypercholesterolaemia) is a genetic disorder characterized by high cholesterol levels, specifically very high low-density lipoprotein (LDL, "bad cholesterol") levels, in the blood and early cardiovascular disease. Many patients have mutations in the LDLR gene that encodes the LDL receptor protein, which normally removes LDL from the circulation, or apolipoprotein B (ApoB), which is the part of LDL that binds with the receptor; mutations in other genes are rare. Patients who have one abnormal copy (are heterozygous) of the LDLR gene may have premature cardiovascular disease at the age of 30 to 40. Having two abnormal copies (being homozygous) may cause severe cardiovascular disease in childhood. Heterozygous FH is a common genetic disorder, occurring in 1:500 people in most countries; homozygous FH is much rarer, occurring in 1 in a million births.
Heterozygous (FH) is normally treated with statins, bile acid sequestrants or other hypolipidemic agents that lower cholesterol levels. New cases are generally offered genetic counseling. Homozygous FH often does not respond to medical therapy and may require other treatments, including LDL apheresis (removal of LDL in a method similar to dialysis) and occasionally liver transplantation.
Recently, Genzyme Corp. and Isis Pharmaceuticals Inc have come up with some intresting results from the drug mipomersen [mipomersen - is an antisense oligonucleotide, with phosphorothioate linkage at 5'- postion and 2'-O-methoxymethyl moety] ( phase 3). As per the claim by the companies, the study met its primary endpoint in an intent-to-treat analysis, with a 25 percent reduction in LDL-cholesterol after 26 weeks of treatment, vs. 3 percent for placebo (p<0.001)>.
The trial met all of its secondary and tertiary endpoints, suggesting that mipomersen may offer potential benefits to patients beyond LDL-C reduction. Patients treated with mipomersen experienced a 27 percent reduction in apolipoprotein B vs. 3 percent for placebo; a 21 percent reduction in total cholesterol vs. 2 percent for placebo; and a 25 percent reduction in non-HDL cholesterol vs. 3 percent for placebo (all p<0.001).>Mipomersen patients’ HDL-C levels increased 15 percent (p=0.035 vs. placebo), which combined with the LDL-C reductions observed, resulted in improved LDL/HDL ratios, a ratio considered an important measure of cardiovascular risk. Mipomersen patients’ LDL/HDL ratios decreased by 34% (p<0.001>Mipomersen a representative of Isis’ leadership in the field of RNA targeted therapeutics will bring a sigh of relief to the sufferers of FH, in the days to come.
I had an opportunity to work with ISIS (as contract R & D, Innovasynth Technologies Limited, Khopoli) and really excited to see the results..
Ref : http://ir.isispharm.com/phoenix.zhtml?c=222170&p=irol-newsArticle&ID=1356364&highlight=
Wednesday, June 9, 2010
Lovastatin: A New Weapon Against Plague?
Thursday, June 3, 2010
Synthetic peptide may regenerate brain tissue in stroke victims
"Neurorestorative therapy is the next frontier in the treatment of stroke." claims Dr. Daniel Morris...
Tuesday, October 18, 2016
High fruit intake during adolescence linked with lower breast cancer risk: But increasing alcohol intake in later life associated with higher risk

Monday, February 23, 2009
Lovastatin for the treatment of degenerative disc disease ?
 Lovastatin is a member of the drug class of statins, used for lowering cholesterol (hypolipidemic agent) in those with hypercholesterolemia and so preventing cardiovascular disease. But recentlyDr. Yang and his research group has come up with new innovative idea that Lovastatin, helps the differentiation of disc cells in vitro.
Lovastatin is a member of the drug class of statins, used for lowering cholesterol (hypolipidemic agent) in those with hypercholesterolemia and so preventing cardiovascular disease. But recentlyDr. Yang and his research group has come up with new innovative idea that Lovastatin, helps the differentiation of disc cells in vitro.Degenerative disc disease is one of the leading sources of back and neck pain. Disc degeneration is part of the normal aging of the spine. In this condition, the spinal discs (the pillow-like pads between the bones) lose their cushioning. When this happens, it can cause persistent pain in the lower back, legs, neck or arms. Treatments for pain can include medications and physical therapy. Sometimes surgery is needed if the pain is severe and keeps a person from participating in everyday activities.
In their quest to discover ways to stop or reverse degenerative disc disease, orthopaedic researchers have been removing disc tissue from patients who are having spine surgery and extracting cells from that tissue for cultivation in vitro (a controlled environment outside of a living organism). They then transfer the cells back into the patient. Shu-Hua Yang, MD, PhD, is part of a Taiwanese research team that has discovered that Lovastatin, a cholesterol-lowering medication, helps the differentiation of disc cells in vitro.
The results are of great interest : 1. the number of nucleus pulposus cells had increased; 2. Lovastatin increased the synthesis of collagen II, a protein that makes up moveable joints, and decreased the synthesis of collagen I, a protein that is related to fibrosis and 3. Lovastatin had no cytotoxicity (the quality of being toxic) on nucleus pulposus cells..
I think if proven, one more addition to the list of serendipity.......
Though further studeis are essential to establish their claim, its a good beginning..
Sunday, September 28, 2014
Rosuvastatin promotes bone growth in mice with achondroplasia symptoms
Saturday, August 21, 2010
Endothelial Function Improvement With Dietary (Cocoa) Flavanols in Patients With Coronary Artery Disease....
A new study by UCSF cardiologists and researchers lead by Dr. Yerem Yeghiazarians found that high concentrations of cocoa flavanols decrease blood pressure, improve the health of blood vessels and increase the number of circulating blood-vessel-forming cells in patients with heart disease. The findings indicate that foods rich in flavanols such as cocoa products, tea, wine, and various fruits and vegetables have a cardio-protective benefit for heart disease patients.
Flavanols are phytonutrient compounds that are found naturally in apples, grapes, tea, cocoa and cherries, which account for the antioxidant effect provided by red wine and green tea. The study found a protective effect from a cocoa drink with 375 mg of flavanols, but according to researchers, a standard or recommended dosage has not yet been defined to achieve optimal health benefit.
The UCSF team has shown for the first time that one of the possible mechanisms of flavanol's benefit is an increase in the circulation of so-called angiogenic cells in the blood. These cells, also known as early endothelial progenitor cells, are critical for the repair process after vascular injury, and perform function and maintenance roles in the endothelium. Endothelium is the thin layer of cells that line the interior wall of blood vessels.
In the current study, the benefit seen from the two-fold increase in circulating angiogenic cells was similar to that achieved by therapy with statins and with lifestyle changes such as exercise and smoking cessation. The benefit demonstrated with cocoa flavanol therapy occurred in addition to the medical regimen already being taken by study participants.
"Our data support the concept that dietary flavanols at the levels provided -- in tandem with current medical therapy -- are safe, improve cardiovascular function, and increase circulating angiogenic cells, which have previously been shown to correlate positively with long-term cardiovascular outcomes" said Yeghiazarians.
Though long-term trials examining the effects of high-flavanol diets on cardiovascular health and function are warranted, but these early findings help us understand how these compounds impact the function of damaged blood vessels...
Ref : Yerem Yeghiazarians et.al., J. Am. Coll. Cardiol., July 13, 2010; 56: A20.




