"As lifestyle programs like the Diabetes Prevention Program are promoted in primary care settings, we hope physicians will integrate and insurers support healthy lifestyle strategies as part of the optimal management of individuals at risk for both new-onset diabetes and cardiovascular disease," the authors write.
Saturday, July 6, 2019
Statin Use Associated With Higher Incidence of Diabetes
Tuesday, January 6, 2015
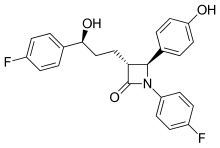
Cholesterol Drug Vytorin Linked to Reduced Heart Attack Risk
Friday, June 17, 2016
Evolocumab could be more effective than ezetimibe in lowering cholesterol in statin-intolerant patients

- In Phase A, patients were assigned to two groups. Each group was treated for 10 weeks with atorvastatin or placebo in a blinded fashion, then crossed over to the alternate therapy for another 10 weeks. Patients were asked to report any muscle pain or weakness.
- Patients who reported intolerable muscle symptoms on atorvastatin, but not placebo, moved to Phase B. In this 24-week phase, patients with confirmed statin intolerance were administered two alternative non-statin therapies, ezetimibe vs. evolocumab.
- The research is being presented at the American College of Cardiology's 65th Annual Scientific Session and simultaneously published online in the Journal of the American Medical Association."Statin intolerance has been a very challenging clinical problem," said Steven Nissen, M.D., chairman of Cardiovascular Medicine at Cleveland Clinic. "The study showed that PCSK9 inhibitors can significantly lower cholesterol in patients with documented statin intolerance, providing an effective treatment for these difficult to manage patients."The GAUSS-3 trial enrolled 511 patients with very high levels of LDL cholesterol - averaging more than 210 mg/dL ¬¬- and with a history of muscle-related statin intolerance. More than 80% of participants had previously reported intolerance to three or more statins. The study showed that 42.6 percent of these patients reported muscle pain or weakness on atorvastatin, but not placebo, and 26.5 percent on the placebo, but not atorvastatin.
Wednesday, March 31, 2021
Statin use alone or with metformin may increase survival in high-risk prostate cancer patients
With respect to prostate mortality, metformin plus statin was associated with a 36% reduction in risk of death followed by statins alone. Those taking metformin alone were relatively rare, and there was no significant association with all-cause mortality."
Friday, January 29, 2021
Statins May Protect Heart From Chemo for Early Breast Cancer
For women with early breast cancer treated with anthracyclines, statin exposure is associated with a lower risk for hospital presentation for heart failure, according to a study published online Jan. 6 in the Journal of the American Heart Association.
Husam Abdel-Qadir, M.D., Ph.D., from the Women's College Hospital in Toronto, and colleagues conducted a retrospective cohort study involving women aged 66 years and older without prior heart failure who received anthracyclines or trastuzumab for newly diagnosed early breast cancer. Using propensity scores, statin-exposed and unexposed women were matched in a 1:1 ratio. Data were included for 666 statin-discordant pairs of anthracycline-treated women and 390 pairs of trastuzumab-treated women.
The researchers found that the five-year cumulative incidence of heart failure hospital presentations after anthracyclines was 1.2 percent (95 percent confidence interval [CI], 0.5 to 2.6 percent) and 2.9 percent (95 percent CI, 1.7 to 4.6 percent) in statin-exposed and unexposed women, respectively (P = 0.01). In the anthracycline cohort, the cause-specific hazard ratio associated with statins was 0.45 (95 percent CI, 0.24 to 0.85; P = 0.01). The five-year cumulative incidence of heart failure hospital presentations after trastuzumab was 2.7 percent (95 percent CI, 1.2 to 5.2 percent) and 3.7 percent (95 percent CI, 2.0 to 6.2 percent) in statin-exposed and unexposed women, respectively (P = 0.09), with a cause-specific hazard ratio associated with statins of 0.46 (95 percent CI, 0.20 to 1.07; P = 0.07).
"This study does not conclusively prove statins are protective," Abdel-Qadir said in a statement. "However, this study builds on the body of evidence suggesting that they may have benefits."
Monday, March 15, 2010
Eprotirome a promising addition to statin therapy ?
Interestingly, the researchers caution that the results don't suggest that eprotirome will or should replace statins, which are the current gold standard for treating high LDL cholesterol.
Thursday, March 14, 2019
Statins Help the Heart, No Matter What Your Age
Cholesterol-lowering statins are already known to help cut heart risks for seniors and the middle-aged. Now, research confirms the meds can also help people aged 75 and older.
"Statin therapy has been shown to prevent cardiovascular disease in a wide range of people, but there has been uncertainty about its efficacy and safety among older people," said lead investigator Anthony Keech. He's a professor of medicine, cardiology and epidemiology at the University of Sydney in Australia.
"Our study summarized all the available evidence from major trials to help clarify this issue. We found that there were significant reductions in major vascular events in each of the six age groups considered, including patients [who were] aged over 75 at the start of treatment," Keech said in an Oxford news release.
"Statin therapy appears to be just as effective in people aged over 75 years as it is in younger people," study co-investigator Jordan Fulcher said in the news release. Fulcher is a cardiovascular research fellow at the University of Sydney.
"We have definitive evidence that statins benefit older people who have suffered a heart attack or stroke. Fewer healthy older people were represented in these trials, so more information in this group of people would help confirm the same benefits that we see in our overall trials population," he said.
"Since the risk of heart attack and stroke increases with age, the potential benefits are likely to be even greater for older people," he said.
"Therefore, there is a need to ensure that patients at risk of cardiovascular disease due to their age are offered statin therapy where there is good reason to believe that it will be beneficial," Baigent said.
Thursday, May 27, 2021
FDA Approves Roszet (rosuvastatin and ezetimibe) to Reduce LDL-C in Hyperlipidemia and Homozygous Familial Hypercholesterolemia
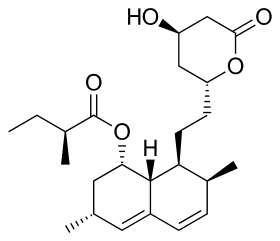
Althera Pharmaceuticals, a company focused on heart health, announced the FDA approval of Roszet (rosuvastatin and ezetimibe) tablets, as an adjunct to diet, for treatment of elevated low-density lipoprotein cholesterol (LDL-C) in adult patients with primary non-familial hyperlipidemia and in adult patients with homozygous familial hypercholesterolemia. Roszet contains rosuvastatin, a powerful statin for LDL-C reduction, and ezetimibe, an efficacious cholesterol absorption inhibitor. The two components work through distinct but complimentary mechanisms to give Roszet the power to significantly lower LDL-C.
“The optimal LDL-C levels in guidelines across the world have been shifting lower and now many patients need to get their LDL-C below 70 mg/dL,” said Dr. Christie Ballantyne, Chief of Cardiology and Cardiovascular Research at Baylor College of Medicine. “These levels can be quite difficult to achieve with just a statin on top of diet and exercise. Rosuvastatin and ezetimibe have been extensively studied in combination therapy and have been shown to significantly reduce LDL cholesterol beyond the statin alone. Combination therapy has been widely used in hypertension to achieve lower blood pressure targets. This new therapy provides a high efficacy statin plus ezetimibe in a single once daily pill which is a powerful new option to help get patients to the desirable LDL goal without increasing pill burden or requiring addition of injectable therapies”
"With Roszet’s approval in the U.S., we reaffirm our commitment to improving cholesterol treatment options for physicians and patients," said Sanjeev Agarwal, CEO of Althera Pharmaceuticals. "We are on a mission to positively impact patients’ health. By making this highly effective medicine available and affordable, we hope to improve the long-term health of patients, including those with prior cardiovascular disease.”
While a patient's out-of-pocket costs will vary depending on insurance status, the Roszet Savings Program aims to reduce co-pays to as little as $20 per month for eligible patients with commercial insurance coverage. Althera is continuing to work with all stakeholders to ensure that Roszet is affordable and accessible to all. Please visit http://www.roszet.com for more information and updates about the Roszet Savings Program and eligibility.
Roszet is available as a once-daily tablet with rosuvastatin/ezetimibe dosages of 5 mg/10 mg, 10 mg/10 mg, 20 mg/10 mg and 40 mg/10 mg.
https://en.wikipedia.org/wiki/Ezetimibe
https://en.wikipedia.org/wiki/Rosuvastatin
Friday, August 14, 2015
Cholesterol-lowering statin drugs could delay prostate cancer growth in patients receiving ADT
Friday, November 1, 2013
New Cholesterol-Lowering Drug, ALN-PCS Shows Early Promise
"Cardiovascular disease remains the leading cause of death of men and women globally and reduction of LDL cholesterol with statin medications has been demonstrated to substantially reduce the risk of first or recurrent cardiovascular events," said Dr. Gregg Fonarow, a professor of cardiology at the University of California, Los Angeles.
Wednesday, January 13, 2021
AHA: Adding Omega-3 Fatty Acids Does Not Cut High CV Risk
In continuation of my update on omega-3 fatty acids
A carboxylic acid formulation of eicosapentaenoic acid and docosahexaenoic acid (omega-3 CA) does not improve outcomes among statin-treated patients at high cardiovascular risk, according to a study published online Nov. 15 in the Journal of the American Medical Association to coincide with the American Heart Association Scientific Sessions 2020, held virtually from Nov. 13 to 17.
Stephen J. Nicholls, M.B.B.S., Ph.D., from Monash University in Melbourne, Australia, and colleagues conducted a double-blind trial comparing omega-3 CA to corn oil in 13,078 statin-treated patients with high cardiovascular risk, hypertriglyceridemia, and low high-density lipoprotein cholesterol from 675 academic and community hospitals in 22 countries. Participants were randomly assigned in a 1:1 ratio to either 4 g/day omega-3 CA or corn oil (6,539 to each) in addition to usual background therapies, including statins.
"These findings do not support use of this omega-3 fatty acid formulation to reduce major adverse cardiovascular events in high-risk patients," the authors write.
Several authors disclosed financial ties to pharmaceutical companies, including AstraZeneca, which funded the study.
Wednesday, January 26, 2022
FDA Approves Leqvio (inclisiran), First-in-Class siRNA to Reduce Low-Density Lipoprotein Cholesterol (LDL-C)
Novartis announced the US Food and Drug Administration (FDA) approval of Leqvio® (inclisiran), the first and only small interfering RNA (siRNA) therapy to lower low-density lipoprotein cholesterol (also known as bad cholesterol or LDL-C) with two doses a year, after an initial dose and one at three months.
"Leqvio is a revolutionary approach to lower LDL-C, and creates new possibilities for how healthcare systems can impact cardiovascular disease, a defining public health challenge of our time," said Vas Narasimhan, Novartis CEO. "We now have the opportunity, working together with partners, to provide this first-ever approved LDL-C–lowering siRNA-based therapy to tackle ASCVD at scale across the United States."
Leqvio is indicated in the United States as an adjunct to diet and maximally tolerated statin therapy for the treatment of adults with clinical atherosclerotic cardiovascular disease (ASCVD) or heterozygous familial hypercholesterolemia (HeFH) who require additional lowering of LDL-C. The effect of Leqvio on cardiovascular morbidity and mortality is being explored in clinical trials currently underway.
"ASCVD is a substantial public health burden affecting 30 million Americans," said Norman Lepor, MD, a Los Angeles based cardiologist and a clinical investigator in the Phase III clinical program for Leqvio. "As a first-of-its-kind siRNA therapy, Leqvio works differently than other cholesterol treatments, with twice-yearly dosing that makes it a compelling option for the millions of people with ASCVD already on cholesterol-lowering medications struggling to reach their LDL-C target."
Leqvio reduces the amount of LDL-C in the bloodstream by improving the liver's natural ability to prevent the production of a protein that plays a role in keeping circulating cholesterol levels high6,7. It is a subcutaneous injection given by a healthcare provider with an initial dose, then again at three months, and then every six months1. This approach may help those who have trouble sticking to medicines that are self-administered and have greater dosing frequency. Leqvio will be available in early January 2022.
"People with ASCVD have most likely experienced a heart attack or stroke from high cholesterol, causing a burden on the family and having a negative impact on lives," said Andrea Baer, Executive Director of The Mended Hearts, Inc. "One of the first steps to improving patients' health is to manage high cholesterol and we're encouraged that this new twice-a-year treatment offers a new option."
The FDA approval was based on results from the comprehensive Phase III ORION-9, -10 and -11 clinical trials, in which all 3,457 participants with ASCVD or HeFH had elevated LDL-C while receiving a maximally tolerated dose of statin therapy2,3. In the Phase III trials at month 17, Leqvio delivered effective and sustained LDL-C reduction of up to 52% vs. placebo and was reported to be well-tolerated with a safety profile shown to be comparable to placebo2,3. The most common side effects were mild to moderate injection site reaction (including pain, redness and rash), joint pain, urinary tract infection, diarrhea, chest cold, pain in legs or arms and shortness of breath2,3.
Novartis has obtained global rights to develop, manufacture and commercialize Leqvio under a license and collaboration agreement with Alnylam Pharmaceuticals, a leader in RNAi therapeutics.
Monday, September 6, 2010
Tuesday, May 17, 2016
PCSK9-inhibitor drugs: A game-changer for individuals with extremely high cholesterol levels
Friday, March 11, 2022
FDA Approves Leqvio (inclisiran), First-in-Class siRNA to Reduce Low-Density Lipoprotein Cholesterol (LDL-C)
"Leqvio is a revolutionary approach to lower LDL-C, and creates new possibilities for how healthcare systems can impact cardiovascular disease, a defining public health challenge of our time," said Vas Narasimhan, Novartis CEO. "We now have the opportunity, working together with partners, to provide this first-ever approved LDL-C–lowering siRNA-based therapy to tackle ASCVD at scale across the United States."
Leqvio is indicated in the United States as an adjunct to diet and maximally tolerated statin therapy for the treatment of adults with clinical atherosclerotic cardiovascular disease (ASCVD) or heterozygous familial hypercholesterolemia (HeFH) who require additional lowering of LDL-C. The effect of Leqvio on cardiovascular morbidity and mortality is being explored in clinical trials currently underway.
"ASCVD is a substantial public health burden affecting 30 million Americans," said Norman Lepor, MD, a Los Angeles based cardiologist and a clinical investigator in the Phase III clinical program for Leqvio. "As a first-of-its-kind siRNA therapy, Leqvio works differently than other cholesterol treatments, with twice-yearly dosing that makes it a compelling option for the millions of people with ASCVD already on cholesterol-lowering medications struggling to reach their LDL-C target."
Leqvio reduces the amount of LDL-C in the bloodstream by improving the liver's natural ability to prevent the production of a protein that plays a role in keeping circulating cholesterol levels high6,7. It is a subcutaneous injection given by a healthcare provider with an initial dose, then again at three months, and then every six months1. This approach may help those who have trouble sticking to medicines that are self-administered and have greater dosing frequency. Leqvio will be available in early January 2022.
"People with ASCVD have most likely experienced a heart attack or stroke from high cholesterol, causing a burden on the family and having a negative impact on lives," said Andrea Baer, Executive Director of The Mended Hearts, Inc. "One of the first steps to improving patients' health is to manage high cholesterol and we're encouraged that this new twice-a-year treatment offers a new option."
The FDA approval was based on results from the comprehensive Phase III ORION-9, -10 and -11 clinical trials, in which all 3,457 participants with ASCVD or HeFH had elevated LDL-C while receiving a maximally tolerated dose of statin therapy2,3. In the Phase III trials at month 17, Leqvio delivered effective and sustained LDL-C reduction of up to 52% vs. placebo and was reported to be well-tolerated with a safety profile shown to be comparable to placebo2,3. The most common side effects were mild to moderate injection site reaction (including pain, redness and rash), joint pain, urinary tract infection, diarrhea, chest cold, pain in legs or arms and shortness of breath2,3.
Novartis has obtained global rights to develop, manufacture and commercialize Leqvio under a license and collaboration agreement with Alnylam Pharmaceuticals, a leader in RNAi therapeutics.
Friday, June 8, 2012
Experimental cholesterol drug, REGN727 (PCSK9 inhibitor) results called ‘game changing
“Wars for PCSK9 are far bigger than the statin wars,” said Dr. Evan A Stein, lead author of the study and researcher at the Metabolic and Atherosclerosis Research Center in Cincinnati, Ohio. “This is a hot research area and everybody is so close together.”
Sunday, September 28, 2014
Rosuvastatin promotes bone growth in mice with achondroplasia symptoms
Saturday, February 23, 2019
Psoriasis Meds Might Help Fight Heart Trouble, Too
"Classically a heart attack is caused by one of five risk factors: diabetes, hypertension, high cholesterol, family history or smoking," explained study lead researcher Dr. Nehal Mehta.
"Our study presents evidence that there is a sixth factor, inflammation," she said.
"The future of cardiovascular prevention may require a cholesterol reduction medication and an anti-inflammatory medication," said Dr. Guy Mintz, who directs heart health at Northwell Health's Sandra Atlas Bass Heart Hospital in Manhasset, N.Y.
"These are exciting times in the area of cardiovascular prevention," said Mintz, who wasn't involved with the study.
"This appears to be an anti-inflammatory effect," Mehta explained in an NHLBI news release. "In the absence of improvement in other cardiovascular risk factors, and without adding new cholesterol medications, patients' soft plaque still improved."
"The best statin in the world can only lower cardiovascular events by approximately 40 percent," Mintz pointed out. "So the question arises, what causes the other 60 percent of cardiovascular events?"
Saturday, July 24, 2010
No Firm Conclusions About HDL Cholesterol Can Be Drawn from JUPITER Sub-Analysis
The European Society of Cardiology (ESC) is concerned that interpretations of a paper about cholesterol, published in the Lancet , could act to deter ongoing research efforts into developing new therapeutic strategies to increase high density lipoprotein (HDL) cholesterol. Caution, the ESC experts advise, should be displayed in the interpretation of the results.....
In the Lancet study, Paul Ridker and colleagues, from Brigham and Women's Hospital (Boston, MA, USA), undertook a retrospective post-hoc analysis of the JUPITER trial. The results show that if a normal, healthy individual has level of low density lipoprotein (LDL), known as "bad cholesterol", substantially lowered with a potent statin, then the level of HDL "good cholesterol" in that person no longer bears any relation to the remaining cardiovascular risk. More.....
Ref : http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2810%2960713-1/fulltext






