Eisai Co., Ltd. (CEO: Haruo Naito, “Eisai”) and Imbrium Therapeutics L.P. (Imbrium Therapeutics), a clinical-stage biopharmaceutical company and operating subsidiary of Purdue Pharma, L.P. (President and CEO: Craig Landau, MD), announced that the U.S. Food and Drug Administration (FDA) has accepted for review the New Drug Application (NDA) for lemborexant, an investigational agent being studied for the treatment of insomnia, a sleep-wake disorder. A Prescription Drug User Fee Act (PDUFA) date is set for December 27, 2019.
The NDA submission was based on data from the clinical development program including two pivotal Phase 3 studies of lemborexant – SUNRISE 1 (Study 304) and SUNRISE 2 (Study 303).
- SUNRISE 1: a one-month Phase 3 clinical study to evaluate the efficacy and safety of lemborexant versus placebo and versus an active comparator (zolpidem tartrate extended release, “zolpidem ER”) in 1,006 patients 55 years and older (45 percent of all patients were aged 65 years and older) with insomnia disorder. This study assessed sleep latency (using latency to persistent sleep; primary objective); sleep efficiency and wake after sleep onset (effect on maintaining sleep; key secondary objectives) objectively using polysomnography, and achieved its primary and key secondary objectives. The most common adverse events (AEs) reported in the lemborexant arms were headache and somnolence.1
- SUNRISE 2: a 12-month placebo-controlled (first six months) Phase 3 clinical study to evaluate the long-term efficacy and safety of lemborexant in 949 adult patients (18 to 88 years of age) with insomnia disorder. This study evaluated subjective (patient-reported) sleep onset latency (primary objective), sleep efficiency, and wake after sleep onset (key secondary objectives) using sleep diaries, and achieved its pre-specified primary and key secondary efficacy objectives. The most common AEs reported in the lemborexant arms were somnolence, nasopharyngitis, headache, and influenza.2
“Our ultimate goal for the development of a sleep-wake treatment is to bring to patients living with insomnia a new option that has the potential to improve their ability to fall asleep, stay asleep and wake the next morning without impairment,” said Lynn Kramer, MD, Chief Clinical Officer and Chief Medical Officer, Neurology Business Group, Eisai. “This milestone for lemborexant brings us one step closer to addressing unmet needs for millions of patients who experience insomnia.”
“Insomnia, a disorder of sleep quality and quantity, causes significant impairment in daily functioning and has long-term consequences for health and well-being,”3 said John Renger, PhD, Vice President, Head of Research & Development and Regulatory Affairs, Imbrium Therapeutics. “We are committed to working with our partner Eisai to make this investigational treatment available to patients, pending regulatory approval.”
Lemborexant is being jointly developed by Eisai and Imbrium Therapeutics for the treatment of multiple sleep-wake disorders, including insomnia disorder. Information about ongoing clinical studies is available at clinicaltrials.gov.
Eisai and Imbrium Therapeutics are striving to address new unmet medical needs and to improve the lives of patients and their families.
This release discusses investigational uses of an agent in development and is not intended to convey conclusions about efficacy or safety. There is no guarantee that such an investigational agent will successfully complete clinical development or gain health authority approval.
About Lemborexant
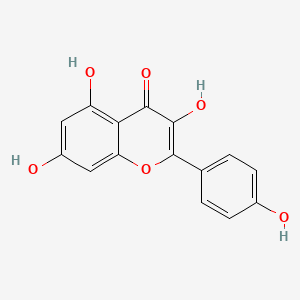
Lemborexant is a novel investigational small molecule compound, discovered and developed by Eisai in-house scientists, that inhibits orexin signaling by binding competitively to both orexin receptor subtypes (orexin receptor 1 and 2). In individuals with normal daily sleep-wake rhythms, orexin signaling is believed to promote periods of wakefulness. In individuals with sleep-wake disorders, it is possible that orexin signaling that regulates wakefulness is not functioning normally, suggesting that inhibiting inappropriate orexin signaling may enable initiation and maintenance of sleep. Eisai and Imbrium Therapeutics are investigating lemborexant as a potential treatment option for multiple sleep-wake disorders, such as insomnia. Additionally, a Phase 2 clinical study of lemborexant in patients with irregular sleep-wake rhythm disorder (ISWRD) and mild to moderate Alzheimer's dementia is underway.
About SUNRISE 1 (Study 304)
SUNRISE 1 was a multicenter, randomized, double-blind, placebo-controlled, active comparator, parallel-group study evaluating the efficacy and safety of lemborexant in 1,006 male or female adult patients 55 years and older (45 percent of patients were 65 years and older) with insomnia disorder conducted in North America and Europe. SUNRISE 1 included a pre-randomization phase of up to 35 days (including a two-week placebo run-in period) and a randomization phase comprised of a 30-day treatment period and a minimum two-week period without treatment prior to the end-of-study visit. In this study, patients were randomized to receive placebo or one of three treatment regimens (lemborexant 5 mg, lemborexant 10 mg, zolpidem ER 6.25 mg).
The primary objective for SUNRISE 1 was to demonstrate using polysomnography that lemborexant at either the 5 mg or 10 mg dose is superior to placebo on objective sleep onset, as measured by latency to persistent sleep after the last two nights of one month of treatment. Key secondary objectives included change from baseline in sleep efficiency and wake after sleep onset (WASO) for both lemborexant doses compared to placebo, and WASO in the second half of the night (WASO2H) for both lemborexant doses compared to zolpidem ER, each after the last two nights of one month of treatment.
About SUNRISE 2 (Study 303)
SUNRISE 2 was a 12-month multicenter, global, randomized, controlled, double-blind, parallel-group study of the efficacy and safety of lemborexant in 949 male or female adult participants 18 to 88 years of age with insomnia disorder. SUNRISE 2 included a pre-randomization phase of up to 35 days (including a two-week placebo run-in period) and a randomization phase comprised of a six-month placebo-controlled treatment period, a six-month period of active-only treatment and a two-week period without treatment prior to the end-of-study visit. In this study, during the placebo-controlled treatment period, patients were randomized to receive placebo or one of two treatment regimens (lemborexant 5 mg or 10 mg). During the active-only treatment period, patients who received placebo during the first period were re-randomized to receive lemborexant 5 mg or 10 mg. Patients who received active treatment during the first period continued on the treatment to which they were originally randomized.
The primary objective was change from baseline in subjective sleep onset latency after six months of placebo-controlled treatment using patient reported (subjective) sleep diaries. Key secondary endpoints were change from baseline in subjective sleep efficiency and subjective wake after sleep onset (sWASO) by using patient reported (subjective) sleep diaries for both lemborexant doses after six months of placebo-controlled treatment.
https://en.wikipedia.org/wiki/Lemborexant