Day One Biopharmaceuticals, Inc. (Nasdaq: DAWN) (“Day One” or the “Company”), a commercial-stage biopharmaceutical company dedicated to developing and commercializing targeted therapies for people of all ages with life-threatening diseases, today announced that the U.S. Food and Drug Administration (FDA) has approved Ojemda (tovorafenib), a type II RAF inhibitor, for the treatment of patients 6 months of age and older with relapsed or refractory pLGG harboring a BRAF fusion or rearrangement, or BRAF V600 mutation. This indication is approved under accelerated approval based on response rate and duration of response. With the approval, Day One received a rare pediatric disease priority review voucher from the FDA.
“Ojemda ushers in a new day for children living with relapsed or refractory pLGG, and we are pleased that we can deliver a new medicine for these patients in desperate need of new treatment options. Moreover, Ojemda is the first and only FDA-approved medicine for children with BRAF fusions or rearrangements, which are the most common molecular alteration in pLGG,” said Jeremy Bender, Ph.D., chief executive officer of Day One. “We are very proud that our first approved medicine addresses this serious and life-threatening disease of childhood and adolescence. We are grateful to the pLGG community, including patients and their families, study investigators, non-profit organizations, and advocacy groups, for their collaboration and support as we strive to close the innovation gap for children with cancer awaiting new treatments.”
pLGG is the most common brain tumor diagnosed in children, with patients suffering profound tumor- and treatment-associated morbidities that can impact their life trajectory. BRAF is the most commonly altered gene in pLGG, with up to 75 percent of children having a BRAF alteration. Until now, there had been no medicines approved for patients with pLGG driven by BRAF fusions.
“pLGG is a chronic and relentless cancer that can devastate children and their families, often stealing their vision, balance and speech,” said Dr. Sabine Mueller, pediatric neuro-oncologist, University of California San Francisco Benioff Children’s Hospitals. “The goal of pLGG treatment is to stabilize or shrink the tumor without further disrupting the child’s and family’s life. Historically, there has been no standard of care for children with pLGG who have relapsed. We are excited to welcome a new targeted treatment option with once-weekly oral dosing designed specifically for these kids and their families.”
Ojemda is the only systemic therapy for pLGG that offers once-weekly dosing, with or without food, as a tablet or oral suspension.



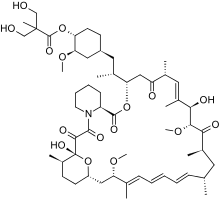 Temsirolimus
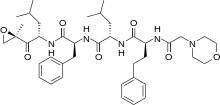
Temsirolimus Ibrutinib
Ibrutinib