In continuation of my update on Ibrutinib

Ibrutinib is a drug for the treatment of rare diseases. It has been approved for the treatment of adults with chronic lymphocytic leukemia (CLL) or with relapsed or refractory mantle cell lymphoma (MCL) since 2014, and since 2015 also for the treatment of adults with Waldenström macroglobulinaemia. Regarding the treatment of patients with CLL or MCL, the Federal Joint Committee (G-BA) already conducted a benefit assessment and made a decision in 2015.
On request of the G-BA, the drug manufacturer now submitted a new dossier because the turnover of the drug in the statutory health insurance exceeded 50 million euros in the preceding 12 months. The German Institute for Quality and Efficiency in Health Care (IQWiG) therefore examined in an early benefit assessment whether the drug offers an added benefit for patients with these diseases in comparison with the respective appropriate comparator therapies.
According to the findings, there is no hint of an added benefit in CLL and Waldenström macroglobulinaemia. In relapsed or refractory mantle cell lymphoma, there is an indication of major added benefit of ibrutinib for patients for whom temsirolimus is the individually optimized treatment option. An added benefit is not proven for patients for whom temsirolimus is no or only a secondary option.
Chronic lymphocytic leukemia
The G-BA differentiated between pretreated and treatment-naive patients within the therapeutic indication of CLL. Pretreated patients were separated into two subpopulations, resulting in three research questions.
Pretreated patients for whom chemotherapy is indicated were to be treated with individually optimized chemotherapy in the comparator arm. The manufacturer presented no relevant data for these patients in its dossier: The direct comparison and the indirect comparisons conducted by the manufacturer were unsuitable for the derivation of an added benefit of ibrutinib.
Pretreated patients for whom such chemotherapy is not an option were to be treated with idelalisib or best supportive care in the comparator arm. A non-quantifiable advantage in the outcome "mortality," but also potentially lesser benefit of ibrutinib in morbidity and health-related quality of life as well as potentially greater harm in severe and serious side effects resulted from the study data presented. In the consideration of the beneficial and harmful effects, an added benefit is therefore not proven for these patients either.
Idelalisib or best supportive care constituted the appropriate comparator therapy also for treatment-naive patients for whom chemo-immunotherapy is unsuitable due to mutations. The manufacturer presented only one study irrelevant for the research question so that an added benefit is not proven for this patient group either.
Waldenström macroglobulinaemia
Pretreated and treatment-naive patients were to be considered separately also in the therapeutic indication Waldenström macroglobulinaemia. In both cases, the appropriate comparator therapy was individually optimized treatment specified by the physician.
The manufacturer presented no data on first-line treatment so that an added benefit of ibrutinib for treatment-naive patients is not proven.
Regarding patients who have received at least one treatment, the manufacturer submitted a historical comparison based on uncontrolled studies because there were no randomized controlled trials. Due to the selective choice of data, among other reasons, this comparison was unsuitable for drawing conclusions on the added benefit. Hence there was no hint of an added benefit in this case either.
Relapsed or refractory mantle cell lymphoma
Two subpopulations have to be differentiated also in relapsed or refractory MCL: patients for whom temsirolimus is the individually optimized treatment, and patients for whom this is not the case.
Due to a lack of data, an added benefit of ibrutinib is not proven for patients for whom temsirolimus is no or only a secondary treatment Option.
For the other patient group, in contrast, the manufacturer presented data from the study MCL3001, in which ibrutinib was compared with temsirolimus. There was no statistically significant difference between the study arms regarding overall survival. Ibrutinib had positive effects in the outcomes "health status" and "side effects," which were not offset by negative effects in other outcomes. Overall, there is therefore an indication of major added benefit for patients for whom temsirolimus constitutes the individually optimized treatment.
G-BA decides on the extent of added benefit
The dossier assessment is part of the early benefit assessment according to the Act on the Reform of the Market for Medicinal Products (AMNOG) supervised by the G-BA. After publication of the dossier assessment, the G-BA conducts a commenting procedure and makes a final decision on the extent of the added benefit.

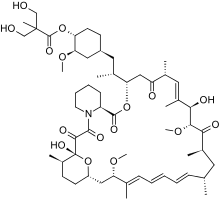 Temsirolimus
Temsirolimus