A team of researchers has found that doses of bilirubin help provide suppression of the immune response following islet transplantation in mouse models. Bilirubin also significantly decreased islet cell death after the cells had been isolated and undergone nutrient deprivation and hypoxic (low oxygen) stress. If applied, the results of the study are expected to improve outcomes after allograft (other donated) islet cell transplantation to treat type 1 diabetes.

Carried out by researchers at North Carolina State University, Ohio State University and the University of California Irvine, the study will be published in a future issue of Cell Transplantation
"Pancreatic islet transplantation has the potential to provide a potentially curative, non-invasive treatment for type 1 diabetes," said Dr. Christopher A. Adin, associate professor, College of Veterinary Medicine, North Carolina State University. "However, stress and injury can cause up to a 70 percent loss of cells in the first 72 hours after transplantation. We hypothesized that bilirubin, an antioxidant, could be used as a supplement to suppress the immune response to allograft islet transplantation. In this study with mice, we administered bilirubin to the pancreas before procurement or added it to a culture after islet isolation."
Bilirubin, a cytoprotectant, has been shown to improve outcomes in cases of sepsis and in solid organ transplantation, said the researchers. The current study, however, is the first to investigate bilirubin as an islet allograft protectant from the immune response and other cell death-causing injury.
The researchers found that bilirubin supplementation could suppress the damage caused by the release of "damage-associated molecular patterns" (DAMPs) that included types of foreign cell-fighting immune cells.
Their studies also revealed that bilirubin also has a direct effect on the phenotype - the physical appearance - of the antigen cells that fight against engraftment, especially macrophages, a type of cell that engulfs and digests cellular debris and foreign substances.
Taken together, that bilirubin can suppress DAMP release, alter cytokine profiles, and affect macrophages, suggests that the use of this natural antioxidant may provide a method for pre-conditioning to improve outcomes after islet allograft transplantation, concluded the researchers.
"With the increasing age of the population, diabetes will increase in prevalence and the demand for new treatment paradigms will become more pressing," said Dr. Camillo Ricordi, Diabetes Research Institute, University of Miami, Miami, FL. "Use of an anti-oxidant compound to combat immune rejection could be an effective method for overcoming obstacles to the advancement of cell therapy for diabetes."
Ref : http://www.ingentaconnect.com/content/cog/ct/pre-prints/content-ct-1616_adin_et_al






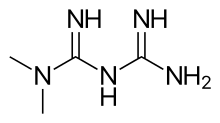 Metformin
Metformin