In continuation of my update on craneberries
In continuation of my update on craneberries
According to the study, recently published by the American Journal of Clinical Nutrition, drinking an 8-ounce (240 ml) glass of cranberry juice a day reduces symptomatic UTIs by nearly 40 percent in women with recurrent UTIs - reducing the burden of UTIs and reducing the antibiotic use associated with treating recurrent UTIs.
"Currently the primary approach to reducing symptomatic events of UTI is the use of chronic antibiotics for suppression, an approach associated with side effects and development of antibiotic resistance. This study shows that consuming one 8-ounce (240 ml) glass of cranberry juice a day reduces the number of times women suffer from repeat episodes of symptomatic UTI and avoids chronic suppressive antibiotics," said Dr. Kalpana Gupta, infectious disease specialist and Professor of Medicine at Boston University's School of Medicine.
An author on the study and panelist at today's session, Dr. Gupta believes that cranberries can help to reduce the worldwide use of antibiotics and significantly improve the quality of life for women who suffer from recurrent UTI symptoms.
Single Largest Clinical Trial on Cranberries of its Kind
The 24-week study of 373 women, conducted by researchers at Boston University, Biofortis Innovation Services (a division of Merieux Nutrisciences) and 18 clinical sites throughout the US and France, is the largest clinical trial of its kind examining the effects of cranberry juice consumption on UTIs. This trial adds to more than 50 years of cranberry research and supports the cranberry's ability to support urinary tract health and reduce symptomatic UTIs among chronic UTI sufferers.
Researchers set out to find whether recurrent (or repeat) UTI sufferers could be protected from repeat infections by drinking cranberry juice. Participants were all healthy women, with an average age of 40, who had experienced at least two UTIs within the past year. During the study, participants were randomly chosen to drink a daily dose of eight ounces (240 ml) of either cranberry juice or a "placebo" beverage without cranberries.
The rate of UTIs decreased significantly among the cranberry drinkers, with just 39 diagnoses during the six-month study compared with 67 in the placebo group.
Compared to some other studies, this trial had greater statistical power to detect differences than others due to its larger sample, use of incidence density to account for the tendency of clinical UTIs to cluster in time within an individual, a high average level of compliance (98%), and a comparatively large percentage of subjects in each group completing the treatment period (86%).
How Cranberries Work
Luckily, cranberries contain a unique combination of compounds including Type-A PACs (or proanthocyanidins) that prevent bacteria from sticking and causing infection. In addition to PACs, new studies have revealed a new class of compounds, xyloglucan oligosaccharides, which have similar anti-bacterial properties against E. coli as PACs. This means there are multiple, unique elements within cranberries working hard for your health.
These unique compounds can be found in a variety of products, including cranberry juice cocktail, 100% cranberry juice, light cranberry juice, dried cranberries and cranberry extract; however most of the research surrounding cranberries and UTIs has been conducted using juice.
Cranberries, a Natural Approach to Better Health
The suggestion that a nutritional approach like cranberry juice could reduce antibiotic use is welcome news given the alarming challenge it presents to public health, one that the WHO refers to as one of the greatest challenges to public health today, and that the UK Chancellor of the Exchequer said could become a threat 'greater than cancer'.
According to Gupta, those who suffer from UTIs can feel confident that this nutritional approach is a potential solution - further validating more than 50 years of well-documented cranberry research.

 Solithromycin
Solithromycin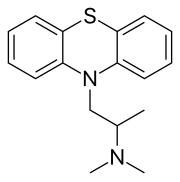 promethazine
promethazine