Basilea Pharmaceutica Ltd, Allschwil (SIX: BSLN), a commercial-stage biopharmaceutical company committed to meeting the needs of patients with severe bacterial and fungal infections, announced today that the US Food and Drug Administration (FDA) approved Zevtera® (ceftobiprole medocaril sodium for injection), for the treatment of adult patients with Staphylococcus aureus bloodstream infections (bacteremia) (SAB), including those with right-sided infective endocarditis, and adult patients with acute bacterial skin and skin structure infections (ABSSSI) and for adult and pediatric patients (3 months to less than 18 years old) with community-acquired bacterial pneumonia (CABP).

David Veitch, Chief Executive Officer of Basilea, said: “We are excited with the US approval of Zevtera. The positive decision by the FDA is a key milestone towards bringing Zevtera to patients in the US. Zevtera has 10 years of market exclusivity from the date of approval and we believe the US provides the most important global commercial opportunity for the brand.”
Dr. Marc Engelhardt, Chief Medical Officer of Basilea, stated: “We are very pleased that the FDA approved Zevtera for all three indications that were submitted with the NDA, including a pediatric labelling. This approval is a landmark for ceftobiprole and reflects its broad clinical utility. The indication in adult patients with Staphylococcus aureus bacteremia, including those with right-sided infective endocarditis, caused by methicillin-susceptible and methicillin-resistant isolates, MSSA and MRSA, addresses a real medical need, as current treatment options are limited.”
The New Drug Application (NDA) was supported by clinical efficacy and safety data from the phase 3 studies ERADICATE (SAB)1 and TARGET (ABSSSI),2 and a phase 3 study in CABP.3 The ERADICATE study was the largest double-blind randomized registrational study conducted for a new antibiotic treatment in SAB.
Vance G. Fowler, Jr., M.D., Professor in the Departments of Medicine and Molecular Genetics & Microbiology at the Duke University School of Medicine and academic lead investigator of the ERADICATE study, commented: “Complicated Staphylococcus aureus infections have a high mortality rate and are associated with substantial morbidity. We need more options for treating these infections, especially if MRSA is involved.”
Thomas Holland, M.D., Associate Professor in the Department of Medicine at the Duke University School of Medicine and chair of the data review committee of the ERADICATE study, added: “There is a high medical need in Staphylococcus aureus bacteremia, therefore, the first approval of a therapy for this indication in over 15 years is highly welcome.”
Adesh Kaul, Chief Financial Officer of Basilea, added: “As we were moving towards completion of the regulatory review, especially with increasing visibility on the expected label, the external interest for commercial partnering increased. Whilst our initial goal was to have announced a commercial partnership by the time of approval of Zevtera in the US, in order to explore fully all potential partnering opportunities, we now expect to complete the process around mid-year. In parallel, we are also taking preparatory steps to shorten the launch timelines, once we have entered into a commercialization partnership.”
Basilea’s phase 3 program for ceftobiprole is funded in part with federal funds from the US Department of Health and Human Services (HHS); Administration for Strategic Preparedness and Response (ASPR); Biomedical Advanced Research and Development Authority (BARDA), under contract number HHSO100201600002C. Through this partnership, Basilea has been awarded approximately USD 112 million, or approximately 75 percent of the costs related to the SAB and ABSSSI phase 3 studies, regulatory activities and non-clinical work.
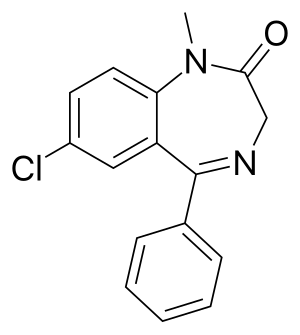
About Zevtera® (ceftobiprole medocaril sodium for injection)
Ceftobiprole, the active moiety of the prodrug ceftobiprole medocaril, is an advanced generation cephalosporin antibiotic for intravenous administration, with rapid bactericidal activity against a wide range of Gram-positive bacteria, such as Staphylococcus aureus, including methicillin-resistant strains (MRSA), and Gram-negative bacteria.4 In several countries in Europe and beyond, the brand is currently approved and marketed as Zevtera® and Mabelio® for the treatment of adult patients with hospital-acquired bacterial pneumonia (HABP), excluding ventilator-associated bacterial pneumonia (VABP), and for the treatment of community-acquired bacterial pneumonia (CABP). Basilea has entered into license and distribution agreements covering more than 80 countries. In the United States, Zevtera is indicated for the treatment of adult patients with Staphylococcus aureus bloodstream infections (bacteremia) (SAB), including right-sided infective endocarditis, and adult patients with acute bacterial skin and skin structure infections (ABSSSI) and for adult and pediatric patients (3 months to less than 18 years old) with community-acquired bacterial pneumonia (CABP).