In continuation of my update on psilocybin

The small feasibility trial, which involved 12 people with treatment-resistant depression, found that psilocybin was safe and well-tolerated and that, when given alongside supportive therapy, helped reduce symptoms of depression in about half of the participants at 3 months post-treatment. The authors warn that strong conclusions cannot be made about the therapeutic benefits of psilocybin but the findings show that more research in this field is now needed.
"This is the first time that psilocybin has been investigated as a potential treatment for major depression," says lead author Dr Robin Carhart-Harris, Imperial College London, London, UK. "Treatment-resistant depression is common, disabling and extremely difficult to treat. New treatments are urgently needed, and our study shows that psilocybin is a promising area of future research. The results are encouraging and we now need larger trials to understand whether the effects we saw in this study translate into long-term benefits, and to study how psilocybin compares to other current treatments."
Depression is a major public health burden, affecting millions of people worldwide and costing the US alone over $200 billion per year. The most common treatments for depression are cognitive behaviour therapy (CBT) and antidepressants. However, 1 in 5 patients with depression do not respond to any intervention, and many relapse.
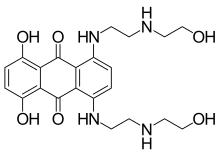
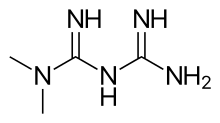
"Previous animal and human brain imaging studies have suggested that psilocybin may have effects similar to other antidepressant treatments," says Professor David Nutt, senior author from Imperial College London "Psilocybin targets the serotonin receptors in the brain, just as most antidepressants do, but it has a very different chemical structure to currently available antidepressants and acts faster than traditional antidepressants."
The trial involved 12 patients (6 women, 6 men) with moderate to severe depression (average length of illness was 17.8 years). The patients were classified as having treatment-resistant depression, having previously had two unsuccessful courses of antidepressants (lasting at least 6 weeks). Most (11) had also received some form of psychotherapy. Patients were not included if they had a current or previous psychotic disorder, an immediate family member with a psychotic disorder, history of suicide or mania or current drug or alcohol dependence.
Patients attended two treatment days -- a low (test) dose of psilocybin 10mg oral capsules, and a higher (therapeutic) dose of 25mg a week later. Patients took the capsules while lying down on a ward bed, in a special room with low lighting and music, and two psychiatrists sat either side of the bed. The psychiatrists were present to provide support and check in on patients throughout the process by asking how they were feeling. Patients had an MRI scan the day after the therapeutic dose. They were followed up one day after the first dose, and then at 1, 2, 3, and 5 weeks and 3 months after the second dose.
The psychedelic effects of psilocybin were detectable 30 to 60 minutes after taking the capsules. The psychedelic effect peaked at 2-3 hours, and patients were discharged 6 hours later. No serious side effects were reported, and expected side effects included transient anxiety before or as the psilocybin effects began (all patients), some experienced confusion (9), transient nausea (4) and transient headache (4). Two patients reported mild and transient paranoia.
At 1 week post-treatment, all patients showed some improvement in their symptoms of depression. 8 of the 12 patients (67%) achieved temporary remission. By 3 months, 7 patients (58%) continued to show an improvement in symptoms and 5 of these were still in remission. Five patients showed some degree of relapse.
The patients knew they were receiving psilocybin (an 'open-label' trial) and the effect of psilocybin was not compared with a placebo. The authors also stress that most of the study participants were self-referred meaning they actively sought treatment, and may have expected some effect (5 had previously tried psilocybin before). All patients had agreement from their GP to take part in the trial. They add that patients were carefully screened and given psychological support before, during and after the intervention, and that the study took place in a positive environment. Further research is now needed to tease out the relative influence of these factors on symptoms of depression, and look at how psilocybin compares to placebo and other current treatments.
Writing in a linked Comment, Professor Philip Cowen, MRC Clinical Scientist, University of Oxford, Oxford, UK, says: "The key observation that might eventually justify the use of a drug like psilocybin in treatment-resistant depression is demonstration of sustained benefit in patients who previously have experienced years of symptoms despite conventional treatments, which makes longer-term outcomes particularly important. The data at 3 month follow-up (a comparatively short time in patients with extensive illness duration) are promising but not completely compelling, with about half the group showing significant depressive symptoms. Further follow-ups using detailed qualitative interviews with patients and family could be very helpful in enriching the assessment."
Ref :http://dx.doi.org/10.1016/S2215-0366(15)00576-3
Ref :http://dx.doi.org/10.1016/S2215-0366(15)00576-3