Allergan plc (NYSE: AGN) announced that the U.S. Food and Drug Administration (FDA) has approved the company's supplemental New Drug Application (sNDA) for Avycaz (ceftazidime and avibactam), expanding the label to include pediatric patients 3 months and older for the treatment of complicated intra-abdominal infections (cIAI) in combination with metronidazole and complicated urinary tract infections (cUTI). This is the first FDA approval of a pediatric indication for cUTI and cIAI in more than a decade.

"Difficult-to-treat gram-negative pathogens pose a significant health risk, particularly to the vulnerable and sensitive pediatric patient population with few options for treatment," said David Nicholson, Chief Research & Development Officer at Allergan. "As resistance rises among the gram-negative pathogens that cause these serious infections, the expanded label for Avycaz provides a safe and effective treatment option now for pediatric patients with cIAI and cUTI. These expanded indications in pediatric patients with infections, including infants and those at a particularly young age, address an unmet need among this vulnerable population and underscore Allergan's efforts in anti-infective research."
The label expansion was approved based on results from two active-controlled clinical studies evaluating Avycaz in children or infants with cIAI or cUTI, as well as a single-dose pharmacokinetic study. In the cIAI study, the safety and efficacy of Avycaz (in combination with metronidazole) was compared with meropenem. In the cUTI study, Avycaz was compared with cefepime.
Across the trials, 128 pediatric patients 3 months to less than 18 years of age were treated with Avycaz. Overall, the findings from the pediatric studies were similar to the previous determination of safety for Avycaz for the treatment of adult patients with cIAI or cUTI, and no new safety concerns were identified in pediatric patients.
The primary objectives of the studies were to evaluate the safety and tolerability of Avycaz, and they were not powered for a statistical analysis of efficacy. The descriptive efficacy analyses in the pediatric studies were consistent with data from studies in adults with cIAI and cUTI. In the pediatric cIAI study, the clinical cure rate at the test-of-cure (TOC) visit in the intent-to-treat (ITT) population was 91.8% (56/61) in the Avycaz plus metronidazole group and 95.5% (21/22) in the meropenem group. Clinical cure rates for the predominant pathogens, Escherichia coli and Pseudomonas aeruginosa, were 90.5% and 85.7%, respectively for patients treated with Avycaz plus metronidazole, and 92.3% and 88.9%, respectively, for patients treated with meropenem. In the pediatric cUTI study, the combined favorable clinical and microbiological response rate at TOC in the microbiological-ITT population was 72.2% (39/54) in the Avycaz group and 60.9% (14/23) in the cefepime group. The microbiologic response rate for E.coli, the most common uropathogen identified in the study, was 79.6% for patients treated with Avycaz and 59.1% for patients treated with cefepime.
Avycaz was first approved by the FDA in February 2015 for the treatment of cUTI including pyelonephritis, and cIAI in combination with metronidazole, caused by designated susceptible bacteria including certain Enterobacteriaceae and P. aeruginosa, for patients 18 years of age and older. Avycaz was subsequently approved for the treatment of adults with hospital-acquired pneumonia / ventilator-associated pneumonia (HABP/VABP) caused by designated susceptible bacteria in February 2018.
About Avycaz (ceftazidime and avibactam)
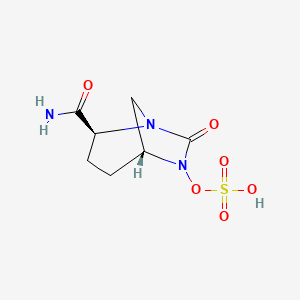
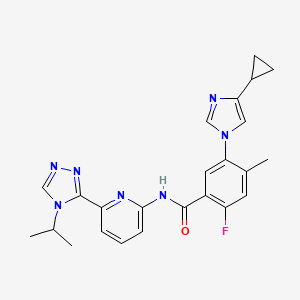
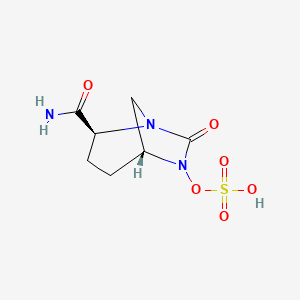
Avycaz is a fixed-dose combination antibacterial indicated for the treatment of cIAI (in combination with metronidazole), and cUTI caused by designated susceptible Gram-negative microorganisms in patients 3 months or older. Avycaz is also indicated for the treatment of hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia (HABP/VABP) in adults. Avycaz consists of a combination of avibactam and ceftazidime.
Avibactam is a first-in-class non-beta-lactam beta-lactamase inhibitor which protects ceftazidime against degradation by certain beta-lactamases. Avibactam does not decrease the activity of ceftazidime against ceftazidime-susceptible organisms. Ceftazadime is a third-generation cephalosporin with a well-established efficacy and safety profile.
Avycaz has demonstrated in vitro activity against Enterobacteriaceae in the presence of some beta-lactamases and extended-spectrum beta-lactamases (ESBLs) of the following groups: TEM, SHV, CTX-M, Klebsiella pneumoniae carbapenemase (KPCs), AmpC and certain oxacillinases (OXA). Avycaz also demonstrated in vitro activity against P. aeruginosa in the presence of some AmpC beta-lactamases, and certain strains lacking outer membrane porin (OprD). Avycaz is not active against bacteria that produce metallo-beta lactamases and may not have activity against Gram-negative bacteria that overexpress efflux pumps or have porin mutations.
Ceftazidime and avibactam is being jointly developed with Pfizer. Allergan holds the rights to commercialize ceftazidime and avibactam in North America under the brand name Avycaz, while Pfizer holds the rights to commercialize the combination in the rest of the world under the brand
Ref : https://www.drugbank.ca/drugs/DB00438
https://en.wikipedia.org/wiki/Ceftazidime
https://en.wikipedia.org/wiki/Avibactam
https://pubchem.ncbi.nlm.nih.gov/compound/Avibactam#section=2D-Structure