In continuation of my updates on depression and its causes
Memory and thinking skills naturally slow with age but now scientists are peeking inside living brains to tell if depression might worsen that decline—and finding some worrisome clues. Depression has long been linked to certain cognitive problems, and depression late in life even may be a risk factor for the development of Alzheimer's. Yet how depression might harm cognition isn't clear.
One possibility: Brain cells communicate by firing messages across connections called synapses. Generally, good cognition is linked to more and stronger synapses. With cognitive impairment, those junctions gradually shrink and die off. But until recently, scientists could count synapses only in brain tissue collected after death.
Yale University scientists used a new technique to scan the brains of living people—and discovered that patients with depression had a lower density of synapses than healthy people the same age.
The lower the density, the more severe the depression symptoms, particularly problems with attention and loss of interest in previously pleasurable activities, Yale neuroscientist Irina Esterlis said Thursday at a meeting of the American Association for the Advancement of Science. She wasn't studying just seniors but a range of ages including people too young for any cognitive changes to be obvious outside of a brain scan—on the theory that early damage can build up.
"We think depression might be accelerating the normal aging," she said.
Her studies so far are small. To prove if depression really worsens that decline would require tracking synaptic density in larger numbers of people as they get older, to see if and how it fluctuates over time in those with and without depression, cautioned Jovier Evans, a staff scientist at the National Institute on Mental Health.
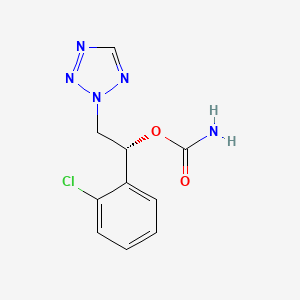
Esterlis is planning a larger study to do that. It's delicate research. Volunteers are injected with a radioactive substance that binds to a protein in the vesicles, or storage bins, used by synapses. Then during a PET scan, areas with synapses light up, allowing researchers to see how many are in different regions of the brain.
Esterlis said there are no medications that specifically target the underlying synapse damage.
But other brain experts said the preliminary findings are a reminder of how important it is to treat depression promptly, so people don't spend years suffering.
"If your mood isn't enough to make you go and get treated, then hopefully your cognition is," said Dr. Mary Sano, who directs the Mount Sinai Alzheimer's Disease Research Center in New York and wasn't involved in the new research.
Still, she cautioned that normal cognitive aging is a complicated process that involves other health problems, such as heart disease that slows blood flow in the brain. It might be that depression, rather than worsening synaptic decline, just makes it more obvious, Sano noted.
With depression "at any age, there's a hit on the brain. At an older age the hit may be more visible because there may already be some loss," she explained.
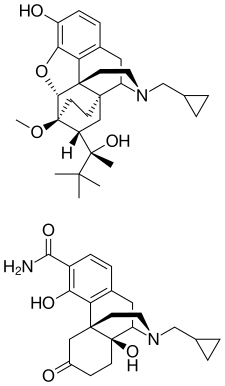
Indeed, another way the brain ages: The blood-brain barrier, which normally protects against infiltration of damaging substances, gradually breaks down, Daniela Kaufer of the University of California, Berkeley, told the AAAS meeting. That triggers inflammation, setting off a cascade that can cause cognitive impairment. Her lab found a specific molecular culprit and is developing, in studies with mice, a way to block the inflammatory damage.
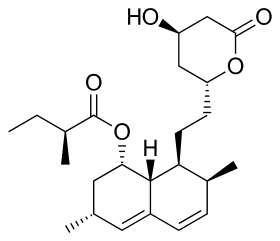
The University of Toronto's Etienne Sibille is developing a compound to target yet another piece of the puzzle, brain receptors that are impaired with both aging and depression. Mouse studies showed it could reverse stress-induced memory loss, he said. Any human testing is at least several years away.
--------------------------------------------------------------------------------------------------------------------------