In continuation of my update on Cabometyx (cabozantinib)
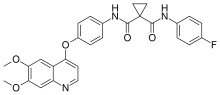
Exelixis, Inc. announced that the U.S. Food and Drug Administration (FDA) approved Cabometyx (cabozantinib) tablets for patients with hepatocellular carcinoma (HCC) who have been previously treated with sorafenib. HCC is the most common form of liver cancer and the fastest-rising cause of cancer-related death in the U.S.
“This new indication for Cabometyx is an important treatment advance for patients with this aggressive form of liver cancer, a community in need of new therapeutic options,” said Michael M. Morrissey, Ph.D., President and Chief Executive Officer of Exelixis. “This approval is an important milestone as we continue to explore how Cabometyx may benefit people with difficult-to-treat-cancers beyond renal cell carcinoma. We would like to thank the patients and clinicians who participated in CELESTIAL and to acknowledge the team at the FDA for their continued collaboration during the review of our application.”
The FDA’s approval of Cabometyx was based on results from the CELESTIAL phase 3 pivotal trial of Cabometyx for patients with advanced HCC who received prior sorafenib. Cabometyx demonstrated a statistically significant and clinically meaningful improvement in overall survival (OS) versus placebo. On November 15, 2018, Exelixis’ partner Ipsen received approval from the European Commission for Cabometyx tablets as a monotherapy for HCC in adults who have previously been treated with sorafenib.
“Patients with this form of advanced liver cancer have few treatment options, particularly once their disease progresses following treatment with sorafenib,” said Ghassan K. Abou-Alfa, M.D., Memorial Sloan Kettering Cancer Center, New York and lead investigator on CELESTIAL. “Physicians are eager for new options for these patients, and the results of the CELESTIAL trial demonstrate that Cabometyx has the efficacy and safety profile to become an important new therapy in our efforts to slow disease progression and improve treatment outcomes.”
In the pivotal CELESTIAL trial, median OS was 10.2 months with cabozantinib versus 8.0 months with placebo (HR 0.76, 95 percent CI 0.63-0.92; p=0.0049). Median progression-free survival (PFS) was more than doubled, at 5.2 months with cabozantinib and 1.9 months with placebo (HR 0.44, 95 percent CI 0.36-0.52; p<0.0001). Objective response rates per RECIST 1.1 were 4 percent with cabozantinib and 0.4 percent with placebo (p=0.0086). Disease control (partial response or stable disease) was achieved by 64 percent of patients in the cabozantinib group compared with 33 percent of patients in the placebo group.
Adverse events in CELESTIAL were consistent with the known safety profile of cabozantinib. The most common (≥10 percent) grade 3 or 4 adverse events in the cabozantinib group compared to the placebo group were palmar-plantar erythrodysesthesia (17 percent vs. 0 percent), hypertension (16 percent vs. 2 percent), increased aspartate aminotransferase (12 percent vs. 7 percent), fatigue (10 percent vs. 4 percent) and diarrhea (10 percent vs. 2 percent). Treatment-related grade 5 adverse events occurred in six patients in the cabozantinib group (hepatic failure, esophagobronchial fistula, portal vein thrombosis, upper gastrointestinal hemorrhage, pulmonary embolism and hepatorenal syndrome) and in one patient in the placebo group (hepatic failure). Sixteen percent of patients in the cabozantinib arm and three percent of patients in the placebo arm discontinued treatment due to treatment-related adverse events.
“While we’ve seen some progress in the treatment of primary liver cancer in recent years, the patient community still needs new and better options,” said Andrea Wilson, President and Founder of Blue Faery: The Adrienne Wilson Liver Cancer Association. “The approval of Cabometyx has been eagerly anticipated, making this an important day for patients diagnosed with this devastating disease.”
In December 2018, Exelixis and its partner Ipsen announced the initiation of COSMIC-312, a phase 3 pivotal trial of cabozantinib in combination with atezolizumab versus sorafenib in previously untreated advanced HCC. The trial will also explore single-agent activity of cabozantinib in the first-line setting. For more information about the trial, visit ClinicalTrials.gov.
https://en.wikipedia.org/wiki/CabozantinibExelixis Announces U.S. FDA Approval of Cabometyx (cabozantinib) Tablets for Previously Treated Hepatocellular Carcinoma