Four new studies surrounding the effects of mango consumption suggest this superfruit has the potential to help combat adverse effects associated with high fat diets and obesity (animal study), as well inhibit growth of fat cells (anti-lipogenic properties in an in-vivo study), slow advancement of breast cancer tumors (animal study), as well as improve regularity and decrease inflammation associated with constipation (human subject study). The research was presented at the 2016 Experimental Biology conference in San Diego.
"While more research is needed, especially in humans, there is a growing body of studies that suggest mango consumption may contribute to some protective effects in relation to obesity, certain cancers, gut health, and inflammation," said Leonardo Ortega, Director of Research at the National Mango Board.
OBESITY
* Nutrition science researcher, Babajide Ojo at Oklahoma State University, was selected by the American Society for Nutrition (ASN) as one of five finalists to present his research at the 2016 ASN Young Minority Investigator Oral Competition. Ojo's study investigated the effects of supplementing mangos (in the form of freeze-dried mango pulp) in mice fed a high fat diet on body composition, glucose homeostasis and gut inflammatory markers.
* Ojo, B., et. al., Mango Supplementation Prevents Gut Microbial Dysbiosis and Modulates Short Chain Fatty Acid Production Independent of Body Weight Reduction in C57BL/6 Mice Fed a High Fat Diet. The FASEB Journal, April 2016, vol. 30 no. 1 Supplement 1166.6 http://tinyurl.
* Chuo Fang, PhD, of the department of Nutrition and Food Science at Texas A&M University investigated the potential role of mango and its microbial metabolites in regulating lipid metabolism and adipogenesis via the activation of AMPK in differentiated 3T3-L1 adipocytes.
* Fang, C., et. al, Mango polyphenols (Mangifera Indica L.) and their microbial metabolites suppress adipogenesis and fat accumulation by mediating AMPK signaling pathways in 3T3L-1 adipocytes. The FASEB Journalvol. 30 no. 1 Supplement 691.10 http://tinyurl.
BREAST CANCER
* Researcher Matt Nemec, of the Interdisciplinary Program of Toxicology at Texas A&M University, studied the anti-proliferative activities of pyrogallol, an intestinal microbial metabolite of gallotannin, a mango polyphenol, on mice with ductal carcinoma in situ breast cancer (DCIS).
* Nemec, M., et. al., Pyrogallol, a microbial metabolites from mango tannins (Mangifera Indica L.) suppresses breast cancer ductal carcinoma in situ proliferation in both in vitro and in vivo. The FASEB Journal, April 2016, vol. 30 no. 1 Supplement 688.7 http://tinyurl.
CONSTIPATION
* Vinicius Paula Venancio, of the Department of Nutrition and Food Science at Texas A&M University, studied the consumption of 300 grams of mango compared to an equivalent amount of fiber (1 teaspoon of a fiber supplement) and its effect on abdominal distention and constipation in otherwise healthy human volunteers.
* Venancio, V.P., et. al., Mango (Mangifera Indica L.) in the promotion of intestinal regularity and decreases inflammation in human subjects with constipation. The FASEB Journal, April 2016, vol. 30 no. 1 Supplement 420.7 http://tinyurl.
Studies show mango consumption may contribute to protective health effects: Four new studies surrounding the effects of mango consumption suggest this superfruit has the potential to help combat adverse effects associated with high fat diets and obesity (animal study), as well inhibit growth of fat cells (anti-lipogenic properties in an in-vivo study), slow advancement of breast cancer tumors (animal study), as well as improve regularity and decrease inflammation associated with constipation (human subject study).








 riluzole
riluzole
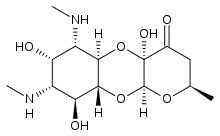
 Apramycin
Apramycin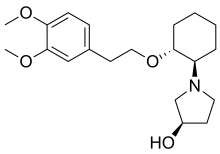 Vernakalant
Vernakalant  Ibutilide
Ibutilide