Showing posts sorted by relevance for query tuberculosis. Sort by date Show all posts
Showing posts sorted by relevance for query tuberculosis. Sort by date Show all posts
Wednesday, May 11, 2011
Wednesday, August 1, 2018
Antimicrobial peptides are promising alternative for combatting antimicrobial resistance
We know that, Antimicrobial peptides (AMPs), also called host defense peptides (HDPs) are part of the innate immune response found among all classes of life. Fundamental differences exist between prokaryotic and eukaryotic cells that may represent targets for antimicrobial peptides. These peptides are potent, broad spectrum antibiotics which demonstrate potential as novel therapeutic agents. Antimicrobial peptides have been demonstrated to kill Gram negative and Gram positive bacteria, enveloped viruses, fungi and even transformed or cancerous cells. Unlike the majority of conventional antibiotics it appears as though antimicrobial peptides may also have the ability to enhance immunity by functioning as immunomodulators.
Antimicrobial peptides are a unique and diverse group of molecules, which are divided into subgroups on the basis of their amino acid composition and structure. Antimicrobial peptides are generally between 12 and 50 amino acids. These peptides include two or more positively charged residues provided by arginine, lysine or, in acidic environments, histidine, and a large proportion (generally >50%) of hydrophobic residues. The secondary structures of these molecules follow 4 themes, including i) α-helical, ii) β-strandeddue to the presence of 2 or more disulfide bonds, iii) β-hairpin or loop due to the presence of a single disulfide bond and/or cyclization of the peptide chain, and iv) extended. Many of these peptides are unstructured in free solution, and fold into their final configuration upon partitioning into biological membranes. It contains hydrophilic amino acid residues aligned along one side and hydrophobic amino acid residues aligned along the opposite side of a helical molecule.. This amphipathicity of the antimicrobial peptides allows them to partition into the membrane lipid bilayer. The ability to associate with membranes is a definitive feature of antimicrobial peptides[ although membrane permeabilization is not necessary. These peptides have a variety of antimicrobial activities ranging from membrane permeabilization to action on a range of cytoplasmic targets.
--------------------------
Overuse of antibiotics has led to the spread of multi-resistant bacteria that do not respond to conventional treatments. Some 700 000 people worldwide die from antimicrobial resistance each year and the future social and economic costs will be huge if nothing is done. New treatment strategies for bacterial infections are desperately needed.
Antimicrobial peptides (AMPs) are a promising alternative for treating infections because they kill bacteria by destroying their enclosing membrane, causing them to disintegrate.
AMPs are fast acting and non-specific; they attack many different bacterial strains. Infectious bacteria are less prone to developing resistance to AMPs, making them an exciting candidate for future treatment strategies.
However, few AMP-based therapies are available because they have low stability – they quickly degrade in storage and during treatment. The challenge is to get AMPs to the site of an infection in the dosage needed and without degradation.
The EU-funded FORMAMP project developed nanotechnology-based carriers to deliver AMPs directly to infected tissue. Encasing AMPs in nanoparticles helped protect them from degradation, with impressive implications.
“FORMAMP showed that structured nanoparticles are efficient delivery vehicles for a range of antimicrobial peptides needed for effective therapy,” explains project coordinator Lovisa Ringstad of RISE, Research Institutes of Sweden.
“Nanoparticles can overcome the major obstacle to peptide-based therapies that promise much in the fight against antimicrobial-resistant infections. For example, in the project we identified highly effective AMPs to combat tuberculosis. This is so promising that we are now seeking collaborators and funding for further development and to move towards eventual clinical testing.”
Fast, controlled delivery
Secondary skin infections in wounds and burns can involve several varieties of infectious bacteria – so a non-specific AMP offers obvious benefits. FORMAMP developed cream and gel formulations that are effective in delivering AMPs to the infected site and releasing them at a controlled rate.
To combat tuberculosis infections, researchers loaded porous silica nanoparticles with specially selected AMPs. Selected nanoparticles also proved very effective in penetrating the bacterial biofilm present in the lungs of cystic fibrosis patients and in wound infections that can act as a significant barrier to otherwise effective treatments.
And the benefits go beyond the ‘magic bullet’ effect of the nanoparticles, says Ringstad. “Most conventional antibiotics are delivered through pills or injections, and if they underperform then more are prescribed. We have focused on treating skin and lung infection locally, thereby reducing exposure and making treatment easier for the patient. Local delivery strategies using nanoparticles can be more cost-effective, as they use less of the active ingredient, and have fewer side effects for the same reason.”
FORMAMP was a proof-of-concept, preclinical laboratory-based project. The researchers explored several nanoparticles, such as porous silica particles, liquid crystaline nanoparticles and dendrimers – star-shaped macromolecules. Desirable properties included non-toxicity and the ability to absorb, protect and release AMPs.
The project examined skin-wound and pulmonary infections, and specialist partners provided a range of AMPs known to work with these conditions.
“One important result concerned the effect of nanoparticles on biofilms,” explains Ringstad. “Biofilms are aggregations of infectious bacteria which protect the infected area against antibiotics and other therapies – they are common in many types of infection and are difficult to penetrate. We found that when nanoparticles are loaded with AMPs then the degradation of the biofilm was significantly improved. This ability to successfully attack biofilms is a very significant result for treating conditions such as cystic fibrosis and burn wound infections.”
The research resulted in many scientific publications and several promising patents that should benefit the SME partners.
Ringstad emphasizes the importance of FORMAMP results. “The nanoparticle delivery mechanism is not limited to treating infections – it could be used in a broad range of therapies. With further research, nanotherapeutics could possibly deliver more effective treatments with fewer side effects and at a lower cost for a wide range of conditions”.
---------------------------------
More at :
Wednesday, February 24, 2010
New insight for design of novel antibiotic derivatives for drug resistant microorganisms...
Viomycin and Capreomycin (a group of nonribosomal peptide antibiotics) belong to the tuberactinomycin (an essential component in the drug cocktail currently used to fight infections of Mycobacterium tuberculosis) Are among the most effective antibiotics against multidrug-resistant tuberculosis. Viomycin was the first member of the tuberactinomycins to be isolated and identified and was used to treat TB until it was replaced by the less toxic, but structurally related compound, Capreomycin. The tuberactinomycins target bacterial ribosomes, binding RNA and disrupting bacterial protein biosynthesis.
Now Dr. Steitz and his colleagues at Yale's Department of Molecular Biophysics and Biochemistry, have identified two structures of tuberactinomycins bound to the ribosome. The researchers claims that, the identification of these structures provides an insight for the design of novel antibiotic derivatives that could be effective against a variety of drug resistant microorganisms.
As per the claim by Dr.Steitz, both antibiotics (Viomycin and Capreomycin) bind to the same site on the ribosome, which lies at the interface between helix 44 of the small ribosomal subunit and helix 69 of the large ribosomal subunit. The structures of these complexes suggest that the tuberactinomycins inhibit translocation by stabilizing the tRNA in the A site in the pretranslocation state. In addition, these structures show that the tuberactinomycins bind adjacent to the binding sites for the paromomycin and hygromycin B antibiotics, which may enable the development of new derivatives of tuberactinomycins that are effective against drug-resistant strains. The authors have presented two crystal structures of the 70S ribosome in complex with three tRNAs and bound to either viomycin or capreomycin at 3.3-and 3.5-Å resolution, respectively in "Nature Structural & Molecular Biology 14 February 2010 ".
Interestingly, Dr. Steitz was awarded the 2009 Nobel Prize in Chemistry for his groundbreaking work determining a high resolution crystal structure of the 50S subunit of the ribosome which has proved to be a major target for antibiotic development.
Hope this discovery will lead to a new insight for design of novel antibiotic derivatives that could be effective against a variety of drug-resistant microorganisms ....
Ref: http://www.rib-x.com/news_and_events/release_2010_02_16
Labels:
antimicrobial,
Capreomycin,
Viomycin
Tuesday, June 30, 2020
New treatment kills off infection that can be deadly to cystic fibrosis patients
A new treatment developed by researchers at Aston University and Birmingham Children's Hospital has been found to completely kill a bacterial infection that can be deadly to cystic fibrosis patients and other chronic lung conditions such as bronchiectasis.
The findings, which are published in the journal Scientific Reports, show that scientists from Aston University, Mycobacterial Research Group, combined doses of three antibiotics—amoxicillin and imipenem-relebactam and found it was 100% effective in killing off the infection which is usually extremely difficult to treat in patients with cystic fibrosis. The infection results in severe decline in lung function and sometimes death.


amoxicillin Imipenem \
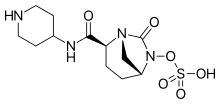 Relebactam
Relebactam
Cystic fibrosis (CF) is a genetic condition affecting more than 10,000 people in the UK (Cystic Fibrosis Trust) and there are more than 70,000 people with the condition worldwide (Cystic Fibrosis Foundation). While bronchiectasis affects 210,000 people in the UK (British Lung Foundation).
Mycobacterium abscessus is a bacterial pathogen from the same family that causes tuberculosis, which causes serious lung infections in people (particularly children) with lung disorders, most notably cystic fibrosis. It is highly drug resistant. Currently patients are given a cocktail of antibiotics that cause serious side effects including severe hearing loss and often doesn't result in cure.
The researchers used samples of the pathogen taken from 16 infected cystic fibrosis patients and tested the new drug combination to discover how much was required to kill the bacteria. They found the amounts of amoxicillin-imipenem-relebactam required were low enough to be given safely to patients.
Until now Mycobacterium abscessus has been virtually impossible to eradicate in people with cystic fibrosis. It can also be deadly if the patient requires a lung transplant because they are not eligible for surgery if the infection is present.
In the UK, of the 10,000 people living with cystic fibrosis, Mycobacterium abscessus infects 13% of all patients with the condition. This new treatment is advantageous not only because it kills off the infection, but it does not have any side-effects on patients, thus ensuring their quality of life and greatly improving survival chances for infected CF patients.
Dr. Jonathan Cox, Lecturer in Microbiology, Aston University and leader of the team that discovered this new treatment said: "This new drug combination is a significant step forward for patients with cystic fibrosis that get infected with the deadly Mycobacterium abscessus bacteria. Our new drug combination is significantly less toxic than those currently used, and so far we have managed to kill every patient's bacterial isolate that we have received.
"This shows our drugs, when used in combination, are widely effective and could therefore make a huge difference to people whose treatment options are currently limited.
"Because amoxicillin is already widely available and imipenem-relebactam has just been approved for use by the Food and Drug Administration (FDA) in the US, these drugs are already available to clinicians. We therefore hope to start treating patients as soon as possible. "
The findings of this research will impact children being treated for the infection at Birmingham Children's Hospital—who part funded the research—but it can also be used nationally and further afield.
With more funding, the next stage of the research will be to test the treatment on more people with CF infected by this bacterium, comparing it to the antibiotics that are currently used.
Dr. Maya Desai, Consultant in Respiratory Paediatrics, Birmingham Children's Hospital added: "This exciting development will significantly impact on the care of CF patients globally. It has been possible only with close collaboration between Aston University and Birmingham Children's Hospital both from a clinical research and financial point of view."
Dr. Paula Sommer, Head of Research at the Cystic Fibrosis Trust said: "It's exciting that these lab-based studies investigating new antibiotic treatments for M. abscessus infection are showing such promise and adding to our expanding knowledge of this devastating bug.
"Mycobacterium abscessus also known as NTM, is the most feared infection a person with cystic fibrosis can develop. Taking drugs to treat NTM can add to an already significant regime of daily treatments and take up to a year to clear infections. We look forward to a time when effective, short courses of treatment are available to treat NTM."
https://en.wikipedia.org/wiki/Amoxicillin
https://en.wikipedia.org/wiki/Imipenem https://en.wikipedia.org/wiki/Relebactam
https://medicalxpress.com/news/2019-10-fda-drug-common-cystic-fibrosis.html
Tuesday, May 7, 2019
TB Medicine Pretomanid Enters Regulatory Review Process in the United States
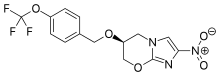
TB Alliance’s new drug application (NDA) for the novel tuberculosis (TB) drug candidate pretomanid has been accepted for review by the United States Food and Drug Administration (FDA). The application is for the use of pretomanid as part of a new regimen, in combination with bedaquiline and linezolid, for the treatment of extensively drug-resistant (XDR) TB, treatment intolerant multidrug-resistant (MDR) TB, and treatment non-responsive MDR-TB.
The NDA for pretomanid has been granted Priority Review by FDA. The Prescription Drug User Fee Act (PDUFA) action date for an FDA decision is in third quarter 2019.
TB Alliance will work with manufacturing partners to ensure that pretomanid, if approved for use in the BPaL regimen, will be accessible to those who need it.
About Pretomanid and the BPaL Regimen
Pretomanid is a new chemical entity and a member of a class of compounds known as nitroimidazooxazines. It has been studied in 20 clinical trials alone or in combination with other anti-TB drugs. Since TB Alliance began development of pretomanid in 2002, it has been administered in a clinical trial setting to more than 1,200 people in 14 countries.
The BPaL regimen (comprised of bedaquiline, pretomanid and linezolid) was first studied clinically in the Phase 3 Nix-TB trial. Nix-TB participants with XDR-TB and treatment intolerant or nonresponsive MDR-TB were enrolled for treatment with the BPaL regimen for six months, extendable to nine months, with the intent to cure. Nix-TB is an open label, single arm trial. According to a modified intention-to-treat analysis of interim results on the first 75 participants presented at the 2018 Union World Conference on Lung Health, 89% of the trial participants had a favorable outcome with their clinical infection resolved and sputum cultures negative for TB after six months of treatment and six months of post-treatment follow-up.
https://www.tballiance.org/portfolio/compound/pretomanid
https://en.wikipedia.org/wiki/Pretomanid
https://www.drugbank.ca/drugs/DB05154
Labels:
Pretomanid,
Regulatory Review Process,
TB,
United States
Tuesday, April 6, 2021
Newly discovered antibiotics kill bacteria differently
Antibiotic resistance is a growing public health problem across the globe, with many diseases becoming harder to treat. Now, a newly discovered antibiotic group shows promise in the fight against superbugs as it has a unique way of killing bacteria.
A team of scientists at McMaster University has found a new group of antibiotics that can fight infections in a new and unique way. These antibiotics fight infections in a way researchers have never seen before, according to the findings of the study described in the journal Nature.
'Holy grail' of antibiotics
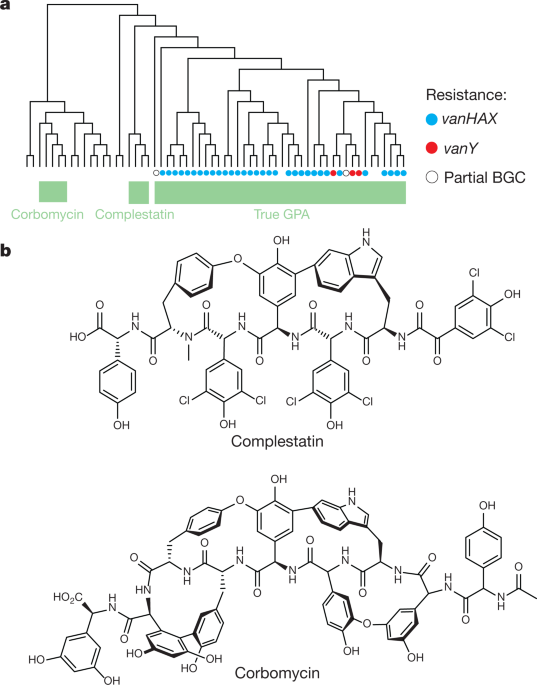
The newly found group of antibiotics, consisting of corbomycin and complestatin, can kill bacteria by blocking the function of the bacterial cell wall. These drugs come from a family of antibiotics known as glycopeptides, which are produced by soil bacteria.
The two antibiotics attack peptidoglycan, the main component of the bacterial cell wall that is vital to the growth and survival of almost all bacteria. They inhibit the action of autolysins, which are important for cell division and growth.
Other antibiotics, such as penicillin, work by preventing the bacteria from building its wall, which is the source of its strength. In killing the bacteria, removing its wall will make it vulnerable and easier to kill.
These new antibiotics work by doing the opposite. Instead of preventing building the wall, it halts the wall ll from being broken down. As a result, blocking the breakdown of the wall would make it impossible for them to divide and expand – just like being trapped in prison.
Unique bacteria killer
The two new antibiotics are known as glycopeptides. The team studied the genes of the group to see if they lack resistance mechanisms. The team believes that if the genes that made these drugs different, perhaps the way they kill will also be different.
In collaboration with scientists from the Université de Montréal, including Yves Brun, they found that the drugs act on the bacterial cell wall to prevent it from dividing and proliferating.
"Knowing the detailed structure at the atomic level of this connection between the surface layer and the surface of the cell offers enormous potential to then develop molecules that can target this attachment and make the cell more sensitive to antibacterials," Yves Brun, study co-author, said.
"Combined with the discovery of the new mode of action of two antibiotics, this development opens up prospects for weakening the action of bacteria and making them more vulnerable," he added.
The researchers believe the group of drugs is a promising clinical candidate in the hopes of stemming bacteria from becoming resistant to antibiotics.
Fight against antibiotic resistance
Antibiotic resistance is one of the greatest threats to global health, according to the World Health Organization (WHO). Though it happens naturally, the misuse of antibiotics is hastening the process, making it easy to treat infections in the past harder to curb now.
Further, antibiotic resistance increase hospital stays and medical costs. For instance, diseases in the past that were responsive to certain antibiotics may become resistant and difficult to stem, such as tuberculosis, pneumonia, gonorrhea, and other infections. Now, as the diseases become stronger and more resilient, outbreaks may become inevitable, unless new drugs are discovered.
In the United States alone, at least 2.8 million people become infected with antibiotic-resistant bacteria each year, while more than 35,000 people die.
https://www.nature.com/articles/s41586-020-1990-9
Monday, August 4, 2014
Researchers uncover how malaria parasite becomes resistant to fosmidomycin drug
Researchers have uncovered a way the malaria parasite becomes resistant to an investigational drug. The discovery, at Washington University School of Medicine in St. Louis, also is relevant for other infectious diseases including bacterial infections and tuberculosis.
The study appears July 24 in Nature Communications.
Many organisms, including the parasite that causes malaria, make a class of molecules called isoprenoids, which play multiple roles in keeping organisms healthy, whether plants, animals or bacteria. In malaria, the investigational drug fosmidomycin blocks isoprenoid synthesis, killing the parasite. But over time the drug often becomes less effective.
"In trials testing fosmidomycin, the malaria parasite returned in more than half the children by the end of the study," said senior author Audrey R. Odom, MD, PhD, assistant professor of pediatrics. "We wanted to know how the parasite is getting around the drug. How can it manage to live even though the drug is suppressing these compounds that are necessary for life?"
Fosmidomycin, an antibiotic, is being evaluated against malaria in phase 3 clinical trials in combination with other antimalarial drugs.
Using next-generation sequencing technology, the research team compared the genetics of malaria parasites that responded to the drug to the genetics of malaria parasites that were resistant to it. With this approach, Odom and her colleagues found mutations in a gene called PfHAD1. With dysfunctional PfHAD1, malaria is resistant to fosmidomycin.
"The PfHAD1 protein is completely unstudied," Odom said. "It's a member of a larger family of proteins, and there are almost no biological functions assigned to them."
In malaria parasites, Odom's team showed that the PfHAD1 protein normally slows down the synthesis of isoprenoids. In other words, when present, PfHAD1 is doing the same job as the drug, slowing isoprenoid manufacturing. Since isoprenoids are necessary for life, it's not clear why the organism would purposefully slow down isoprenoid production.
Ref : http://www.nature.com/ncomms/2014/140724/ncomms5467/full/ncomms5467.html
Thursday, January 23, 2020
FDA Approves Rinvoq (upadacitinib), an Oral JAK Inhibitor for the Treatment of Moderate to Severe Rheumatoid Arthritis
In continuation of my update on Rinvoq (upadacitinib)

AbbVie (NYSE: ABBV), a research-based global biopharmaceutical company, today announced that the U.S. Food and Drug Administration (FDA) has approved Rinvoq (upadacitinib), a 15 mg, once-daily oral Janus kinase (JAK) inhibitor, for the treatment of adults with moderately to severely active rheumatoid arthritis (RA) who have had an inadequate response or intolerance to methotrexate (MTX-IR).1 Rinvoq is expected to be available in the U.S. in late August 2019.
The FDA approval of Rinvoq is supported by data from the SELECT program, one of the largest registrational Phase 3 programs in RA with approximately 4,400 patients evaluated across all treatment arms in five studies.2-6 The studies include assessments of efficacy, safety and tolerability across a variety of RA patients, including those who failed or were intolerant to biologic disease-modifying anti-rheumatic drugs and who were naïve or inadequate responders to methotrexate. Rinvoq is not indicated for methotrexate-naïve patients.
"Despite the availability of multiple treatment options with varying mechanisms of action, many patients still do not achieve clinical remission or low disease activity—the primary treatment goals for rheumatoid arthritis," said Roy M. Fleischmann, M.D., primary investigator for SELECT-COMPARE and clinical professor at the University of Texas Southwestern Medical Center at Dallas. "With this FDA approval, Rinvoq has the potential to help additional people living with RA achieve remission who have not yet reached this goal."
Across the SELECT Phase 3 studies, Rinvoq met all primary and ranked secondary endpoints. The primary endpoints include:
- In SELECT-EARLY, 52 percent of MTX-naïve patients treated with Rinvoq 15 mg achieved ACR50 vs 28 percent treated with MTX at week 121
- In SELECT-MONOTHERAPY, 68 percent of MTX-IR patients treated with Rinvoq 15 mg achieved ACR20 vs 41 percent treated with continued MTX at week 141
- In SELECT-COMPARE, 71 percent of MTX-IR patients treated with Rinvoq 15 mg plus MTX achieved ACR20 vs 36 percent treated with placebo plus MTX at week 121
- In SELECT-NEXT, 64 percent of csDMARD-IR patients treated with Rinvoq 15 mg plus csDMARDs achieved ACR20 vs 36 percent treated with placebo plus csDMARDs at week 121
- In SELECT-BEYOND, 65 percent of biologic-IR patients treated with Rinvoq 15 mg plus csDMARDs achieved ACR20 vs 28 percent treated with placebo plus csDMARDs at week 121
"The discovery and development of Rinvoq is indicative of AbbVie's long-standing commitment to advancing the science for people living with immune-mediated conditions," said Michael Severino, M.D., vice chairman and president, AbbVie. "Today's FDA approval marks an important milestone in our pursuit to deliver innovative medicines that advance care for people living with rheumatoid arthritis."
Clinical Remission
Patients taking Rinvoq achieved clinical remission, a state characterized by almost no disease activity and symptoms, even without methotrexate.2-3,6 Approximately 30 percent of patients treated with Rinvoq achieved clinical remission (as assessed by DAS28-CRP<2.6) at week 12 in SELECT-COMPARE and week 14 in SELECT-MONOTHERAPY compared to six percent with placebo plus methotrexate and eight percent with methotrexate, respectively.1 In SELECT-EARLY, 36 percent of patients treated with Rinvoq achieved clinical remission (as assessed by DAS28-CRP<2.6) at week 12 compared to 14 percent with methotrexate.1
Durable remission rates were observed up to week 26. Forty-eight percent of patients treated with Rinvoq alone in SELECT-EARLY and 41 percent of patients treated with Rinvoq plus methotrexate in SELECT-COMPARE achieved clinical remission at weeks 24 and 26, compared to nine percent with placebo plus methotrexate and 18 percent with methotrexate, respectively.1 Analysis at weeks 24 and 26 were not controlled for multiple comparisons.3,10
Radiographic Inhibition
Rinvoq significantly inhibited radiographic progression as measured by the change in modified total Sharp score (mTSS) from baseline compared to methotrexate in SELECT-EARLY (0.14 vs 0.67) and Rinvoq plus methotrexate compared to placebo plus methotrexate in SELECT-COMPARE (0.15 vs 0.78) through weeks 24 and 26, respectively.1
Safety
The most common side effects associated with Rinvoq include upper respiratory tract infections (common cold, sinus infections), nausea, cough and pyrexia.1 Patients treated with Rinvoq are at increased risk for developing serious infections that may lead to hospitalization or death. These infections include tuberculosis (TB), invasive fungal, bacterial, viral, and other infections due to opportunistic pathogens. Most patients who developed these infections were taking concomitant immunosuppressants such as methotrexate or corticosteroids.1 Lymphoma and other malignancies have been observed in Rinvoq-treated patients.1 Thrombosis, including deep vein thrombosis, pulmonary embolism, and arterial thrombosis, have occurred in patients treated with JAK inhibitors used to treat inflammatory conditions.1 Patients treated with RINVOQ also may be at risk for other serious adverse reactions, including gastrointestinal perforations, neutropenia, lymphopenia, anemia, lipid elevations, liver enzyme elevations, and embryo-fetal toxicity.1
Ease of Use and Access
Designed to help accommodate the physical limitations of people living with RA, the packaging for Rinvoq includes a bottle cap with a wide, easy-to-grip texture and an embedded tool that punctures the foil liner to simplify medication access. This packaging design was awarded the Arthritis Foundation Ease of Use Commendation.
"Rheumatoid arthritis can have a debilitating impact on the lives of those with the chronic disease, including making it difficult to perform everyday tasks," said Cindy McDaniel, senior vice president, consumer health, Arthritis Foundation. "The Arthritis Foundation is committed to recognizing innovation that can help patients living with rheumatoid arthritis and we are proud to recognize AbbVie with our Ease of Use Commendation for the packaging design of Rinvoq."
AbbVie continues to work closely with key stakeholders to support patient access to Rinvoq, including offering a patient support program and a co-pay card that may reduce out-of-pocket costs to $5 per month for eligible, commercially-insured patients. For those with limited or no health insurance, AbbVie offers myAbbVie Assist, a patient assistance program that provides Rinvoq to qualifying patients.
https://en.wikipedia.org/wiki/Upadacitinib
https://www.drugbank.ca/drugs/DB15091
Wednesday, January 10, 2018
New small-molecule drug restores brain function, memory in mouse model of Alzheimer's disease
In continuation of my update on canola oil
An international team of researchers has shown that a new small-molecule drug can restore brain function and memory in a mouse model of Alzheimer's disease. The drug works by stopping toxic ion flow in the brain that is known to trigger nerve cell death. Scientists envision that this drug could be used to treat Alzheimer's and other neurodegenerative diseases such as Parkinson's and ALS.
An international team of researchers has shown that a new small-molecule drug can restore brain function and memory in a mouse model of Alzheimer's disease. The drug works by stopping toxic ion flow in the brain that is known to trigger nerve cell death. Scientists envision that this drug could be used to treat Alzheimer's and other neurodegenerative diseases such as Parkinson's and ALS.
"This is the first drug molecule that can regulate memory loss by directly blocking ions from leaking through nerve cell membranes," said Ratnesh Lal, a professor of bioengineering at the University of California San Diego and co-senior author of the study.
Various studies have linked Alzheimer's disease to the accumulation of two particular proteins in the brain called amyloid-beta and tau. One theory is that these protein clusters create pores in nerve cell membranes that allow ions to travel in and out uncontrollably. This would alter ion levels inside the cells and in turn trigger neuronal dysfunction and cell death.
The new drug, a small molecule called anle138b, blocks these pores from moving ions in and out of nerve cells. Anle138b attaches to both amyloid-beta and tau protein clusters and deactivates the pores created by these clusters.
Researchers administered anle138b to mice with a genetic predisposition for developing an Alzheimer's-like condition. The mice had symptoms such as abnormal brain function, impaired memory and high levels of either amyloid-beta or tau proteins in the brain. Treatment with anle138b normalized brain activity and improved learning ability in mice.
The study was led by the German Center for Neurodegenerative Diseases, the University Medical Center Göttingen, the Braunschweig University of Technology, the Max Planck Institute for Biophysical Chemistry, the Center for Nanoscale Microscopy and Molecular Physiology of the Brain in Göttingen, Germany, and the University of California San Diego. Researchers published their findings on Dec. 5 in EMBO Molecular Medicine.
Christian Griesinger, a professor at the Max Planck Institute for Biophysical Chemistry and co-senior author of the study, noted, "The drug is able to reach the brain when taken orally. Therefore, it is easy to administer, and we are currently performing toxicology studies to eventually be able to apply anle138b to humans."
The team cautions that since the drug has so far only been tested in mice, it is unclear how well it would perform in humans. "I would like to emphasize that none of the current animal models fully recapitulate the symptoms seen in Alzheimer's patients. Thus, care has to be taken when interpreting such data. However, our study offers evidence that anle138b has potential for neuroprotection," said André Fischer, a senior researcher at the German Center for Neurodegenerative Diseases and the University Medical Center Göttingen, who is also a co-senior author of the study.
While collaborators in Germany will be pursuing clinical studies in human patients with neurodegenerative diseases, Lal and his research group at the UC San Diego Jacobs School of Engineering are particularly interested in testing anle138b on a variety of other diseases that are linked to toxic ion flow caused by amyloid proteins, including diabetes, tuberculosis and certain types of cancer. Lal's group has performed extensive research on amyloid ion channels and their roles in these diseases. "Blocking the ion leakiness of amyloid channels using anle138b could be an effective therapy for various diseases," Lal said.
Lal serves as co-director for the Center of Excellence for Nanomedicine and Engineering, a subcenter of the Institute of Engineering in Medicine at UC San Diego. His research group will also work on targeted delivery of the drug using their patent pending "nanobowls," which are magnetically guided nanoparticles that can be packed with drugs and diagnostic molecules, deliver them to particular sites in the body and release them on demand. Future studies will focus on using these nanobowls to deliver anle138b to the brain, as well as other diseased tissues and organs affected by toxic amyloid-beta ion channels.
http://ucsdnews.ucsd.edu/pressrelease/experimental_drug_block_toxic_ion_flow_linked_to_alzheimers_disease
Sunday, January 24, 2010
New class of drugs for hepatitis C .....
Eiger BioPharmaceuticals, Inc., has come up with a novel class of compounds as HCV Inhibitors. The research validates a domain, termed 4BAH2, within the non-structural protein (NS4B) of the HCV genome, as essential for HCV replication and describes the development of a high-throughput screen leading to the identification of small molecule inhibitors of 4BAH2.
Interestingly, the researchers claims that 4BAH2 is the second new domain within NS4B now proven necessary and essential for HCV replication, and which has been shown to be susceptible to pharmacologic inhibition. Eiger is developing small molecule inhibitors of both NS4B-RNA binding and small molecule inhibitors of NS4B-AH2, each of which has significant activity alone and significant synergy when combined. The researchers have tried the following two compounds (a pyrazolopyrimidine derivative and an amiloride derivative see the below structures). Mechanistic studies reveal that the inhibitors target 4BAH2 function by preventing either 4BAH2 oligomerization or 4BAH2 membrane association. 4BAH2 inhibitors represent an additional class of compounds with potential to effectively treat HCV.
Eiger is focused on the discovery and development of new antiviral agents against novel targets for the treatment of hepatitis virus infections. Eiger's pipeline includes repurposed clinical stage therapeutic agents as well as preclinical NCEs from discovery that exhibit antiviral activity against Hepatitis C, Hepatitis D, and other viruses.
Ref : http://stm.sciencemag.org/content/2/15/15ra6.abstract
Wednesday, September 5, 2018
FDA Approves Olumiant (baricitinib) 2 mg Tablets for the Treatment of Adults with Moderately-to-Severely Active Rheumatoid Arthritis
Eli Lilly and Company (NYSE: LLY) and Incyte Corporation (NASDAQ: INCY) announced today that the U.S. Food and Drug Administration (FDA) has approved the 2-mg dose of Olumiant (baricitinib), a once-daily oral medication for the treatment of adults with moderately-to-severely active rheumatoid arthritis (RA) who have had an inadequate response to one or more tumor necrosis factor (TNF) inhibitor therapies. Use of Olumiant in combination with other Janus kinase (JAK) inhibitors or biologic disease-modifying antirheumatic drugs (bDMARDs), or with potent immunosuppressants such as azathioprine and cyclosporine is not recommended. Olumiant may be used as monotherapy or in combination with methotrexate (MTX) or other non-biologic DMARDs.

"We are pleased to provide RA patients in the U.S. an effective treatment option with Olumiant, as people with RA who have had an inadequate response to TNF inhibitors are generally considered to be some of the most difficult to treat RA patients," said Christi Shaw, president, Lilly Bio-Medicines.
The Olumiant clinical trial program included the RA-BEACON study, a randomized, double-blind, placebo-controlled study in which patients were randomly assigned to receive Olumiant 2 mg, baricitinib 4 mg or placebo, in addition to conventional DMARDs that they were currently using. This study included 527 patients who had an inadequate response or intolerance to one or more TNF inhibitor therapies. Patients could have had prior therapy with other bDMARDs.
The study results showed that significantly higher ACR20 response rates and improvement in all individual ACR20 component scores were observed at Week 12 with Olumiant.1 The study found that patients treated with Olumiant had significantly higher rates of ACR20 response versus placebo-treated patients at Week 12 (49% of Olumiant-treated patients versus 27% of placebo-treated patients).1Olumiant also demonstrated early symptom relief, with ACR20 responses seen as early as Week 1.1Patients treated with Olumiant reported significant improvements in physical function based on the Health Assessment Questionnaire Disability Index (HAQ-DI) (recording an average score of 1.71 before treatment and 1.31 at Week 12) compared to placebo-treated patients (who recorded an average score of 1.78 before treatment and 1.59 at Week 12).
Olumiant is approved with a Boxed Warning for the risk of serious infections, malignancies and thrombosis. Serious infections leading to hospitalization or death, including tuberculosis and bacterial, invasive fungal, viral, and other opportunistic infections, have occurred in patients receiving Olumiant. Lymphoma and other malignancies have been observed in patients treated with Olumiant as well. Additionally, thrombosis, including deep venous thrombosis, pulmonary embolism and arterial thrombosis, some fatal, have occurred in patients treated with Olumiant. Other warnings and precautions include gastrointestinal perforations, laboratory abnormalities (including neutropenia, lymphopenia, anemia, liver enzyme elevations, and lipid elevations) and a warning against the use of live vaccines with Olumiant. The most common adverse events (occurring in greater than or equal to 1% of Olumiant 2 mg- and baricitinib 4 mg-treated patients in placebo-controlled trials) included upper respiratory tract infections, nausea, herpes simplex and herpes zoster.
As part of the approval, the companies have agreed to conduct a randomized controlled clinical trial to evaluate the long-term safety of baricitinib in patients with rheumatoid arthritis.
"Despite the advancements we've seen in the RA treatment landscape over the past several decades, many patients are still failing to achieve their disease management goals," said Seth Ginsberg, co-founder and president of CreakyJoints and the Global Healthy Living Foundation. "As it's important for RA patients to have multiple treatment options available to best suit their disease characteristics and experiences, the approval of Olumiant is very encouraging for our community."
RA is a chronic, painful and progressive form of arthritis It is estimated that about two-thirds of established RA patients will not reach clinical remission with their first TNF inhibitor therapy, and a significant percentage will not maintain efficacy as time goes on.
"In my clinical practice, I continue to see patients who experience debilitating symptoms and who are waiting for a medicine that may be right for them," said Elizabeth L. Perkins, M.D., Rheumatology Care Center, Birmingham, Alabama. "Olumiant is an important option for rheumatologists to help address these patients' unmet needs."
"RA patients continue to experience unique challenges accessing the treatments prescribed by their healthcare providers. Therefore, we are determined to continue our work with stakeholders to demonstrate value across the healthcare system so providers have greater choice in prescribing treatments to fit individual patient needs," said Shaw.
Lilly will launch Olumiant in the U.S. by the end of the second quarter of 2018. The price of Olumiant will be 60% less than the leading TNF inhibitor.5 Lilly will be offering a patient support program, Olumiant Together™. For more information about this program, please call 1-844-Olumiant.
Incyte is now eligible to receive a $100 million milestone payment from Lilly as a result of the Olumiant approval, which Incyte expects to recognize in the second quarter of 2018.
Saturday, April 10, 2010
UT Southwestern researchers find clues to TB drug resistance.....
In continuation of my update on TB and its challenges...
Now researchers from the University of Texas Southwestern Medical Center at Dallas, have come up with some interesting info. i.e., a type of blood pressure medication shows promise at overcoming some drug-resistant tuberculosis, at least in the laboratory.
Dr. Gumbo (lead researcher) and his colleagues used an experimental apparatus to simulate the way TB bacteria grow in the human lung. When they exposed the bacteria to drugs commonly used to treat the disease (ethambutol and isoniazid), the bacterial cells activated a cellular mechanism that pumps each drug out of the cells.
"The pumping action enables the rapid emergence of high-level resistance to the drugs whether administered together as well as individually, Dr. Gumbo said".
As per the claim by the researchers, resistance was drastically reduced when the researchers gave the blood-pressure drug reserpine – which is known to block this pumping action – to the TB cells before administering ethambutol and isoniazid.
Researchers now want to test all the first-line drug treatments together with the pump blocker in humans. Hope they will come up with positive results.....
Researchers now want to test all the first-line drug treatments together with the pump blocker in humans. Hope they will come up with positive results.....
Ref : http://www.utsouthwestern.edu/utsw/cda/dept37389/files/582308.html
Sunday, January 31, 2010
Rapamycin as a potential treatment for kidney disease (ADPKD).........
I did mention about the use of Rapamycin (see structure) to improve the efficacy of tuberculosis vaccine in my earlier blog. This drug has been already used as an immunosuppressant drug to prevent rejection in organ transplantation, especially useful in kidney transplants.
Rapamycin, was originally developed as an antifungal agent. However, this was abandoned when it was discovered that it had potent immunosuppressive and antiproliferative properties. Some researchers have also reported that the drug prolong the life of mice and might also be useful in the treatment of certain cancers.
Researchers from UC Santa Barbara earlier claimed that, rapamycin has a potential to treat kidney disease, however concluded that the mice had different genes affected than human patients. Interestingly, the same researchers recently found that "rapamycin is also highly effective in a new mouse model in which the same gene is affected as in most human patients".
As claimed by the lead researcher, Thomas Weimbs currently, no treatment exists to prevent or slow cyst formation and most ADPKD patients require kidney transplants or lifelong dialysis for survival. I think this will boost the confidence of the several international groups, who are undertaking the clinical trials to test the safety and efficacy of rapamycin and related drugs in polycystic kidney disease. Though the researchers are hopeful of positive results they caution that, it will be critical to balance any benefits against the expected side effects to judge whether these drugs should be recommended for the treatment of polycystic kidney disease. Let us be optimistic.....
Ref : http://www.ia.ucsb.edu/pa/display.aspx?pkey=2164
Labels:
ADPKD,
polycystic kidney disease,
Rapamycin
Wednesday, January 14, 2009
A new avenue for TB therapy !
TB bacteria actually sends signals that encourage the growth of those organized granuloma structures, and for good reason: each granuloma serves as a kind of hub for the infectious bugs in the early stages of infection, allowing them to expand further and spread throughout the body. Which is something interesting in he sense that the earlier believed fact (i.e., masses of immune cells that form as a hallmark of tuberculosis (TB) have long been thought to be the body's way of trying to protect itself by literally walling off the bacteria) is being ruled out?. Scientists thought they were protective, but they are not - at least not in early infection. The bacteria use them to reproduce and disseminate themselves.
Not only do the bacteria expand themselves within the first granuloma to form, she added, but some of the immune cells in that initial mass leave to start new granulomas elsewhere. Those new granulomas then also serve as breeding grounds for the bacteria. The finding (Lalita Ramakrishnan and J.Davis). suggests a new avenue for TB therapy at an important time in the struggle against TB infection (not only the increasing number of patients, AIDS with TB and drug resistant TB). So if one can prevent granulomas that might be therapeutic either by intercepting the bacterial signal that spurs granulomas' formation or by manipulating the human immune system in some other way. Hope this research will go a long way in finding the solution to the epidemic drug resistant TB........
Not only do the bacteria expand themselves within the first granuloma to form, she added, but some of the immune cells in that initial mass leave to start new granulomas elsewhere. Those new granulomas then also serve as breeding grounds for the bacteria. The finding (Lalita Ramakrishnan and J.Davis). suggests a new avenue for TB therapy at an important time in the struggle against TB infection (not only the increasing number of patients, AIDS with TB and drug resistant TB). So if one can prevent granulomas that might be therapeutic either by intercepting the bacterial signal that spurs granulomas' formation or by manipulating the human immune system in some other way. Hope this research will go a long way in finding the solution to the epidemic drug resistant TB........
Labels:
Drug Discovery,
Medicinal Chemistry,
Tuberculosis
Sunday, January 25, 2009
Use of Liquid crystals in high-resolution digital X-rays !
We have seen many applications of liquid crystals, but now something interesting like "X-ray light valve" (a term coined by Dr.John Rowlands). This finds importance because the use of liquid crystals reduces the cost of high-resolution digital X-rays by many folds. As the use of digital X rays is becoming essential (because its simple to analyse, manipulate and store-in comparison with the presently used ones). Most of them work by using a layer of amorphous selenium to convert the X-rays into electric charge. This charge image is then recorded using an array of transistors and other electronic components, akin to those used in some digital cameras.
X-rays cannot be easily focused, so X-ray machines work by recording the shadow of an object rather than a focused image. That means the recording medium, be it an electronic imager or conventional X-ray film, must be at least the same size as the object being scanned and this add to the cost of digitally imaging. Thanks to Dr.Rowland and his group for X-ray light valve-consisting of a layer of liquid crystal - which is opaque or transparent depending on whether an electric charge is present - covered with a layer of amorphous selenium. These layers are sandwiched between a pair of electrodes which generate an electric field across them. When an X-ray is taken, the rays that hit the selenium layer generate a charge which is drawn towards the liquid crystal by the electric field. This makes the liquid crystal transparent at those locations. The overall pattern of transparency and opacity can be read off the liquid crystal layer using a light-based digital scanner and presented as a digital image. This research is of significance because of the fact that it separates the read-out system from the X-ray mechanism.
As pulmonary tuberculosis is becoming an epidemic in the developing countries, development of this technique is a boon to the people.
When I was working for my Ph.D., my guide (Dr. Shankar C. Bennur (now retired) Professor of Organic Chemistry, Karnatak University Dharwad, Karnatak, India) used to tell me that the liquid crystals will have many fold uses in the days to come. He did work (UFSC, Florianopolis, SC, Brazil) on the synthesis of many liquid crystals and used to tell me about his experience with this interesting field (which was at nascent stage). Whenever we used to get products (in my case, the compounds had methylene aminoxy methyl moiety) with low melting points, he used to elaborate about smectic point./long chain compounds.....Hope, he will be happy about this innovative idea. Congrats Dr.Rowland......
Ref : http://www.allbusiness.com/medicine-health/diseases-disorders-respiratory-disease/12124600-1.html
X-rays cannot be easily focused, so X-ray machines work by recording the shadow of an object rather than a focused image. That means the recording medium, be it an electronic imager or conventional X-ray film, must be at least the same size as the object being scanned and this add to the cost of digitally imaging. Thanks to Dr.Rowland and his group for X-ray light valve-consisting of a layer of liquid crystal - which is opaque or transparent depending on whether an electric charge is present - covered with a layer of amorphous selenium. These layers are sandwiched between a pair of electrodes which generate an electric field across them. When an X-ray is taken, the rays that hit the selenium layer generate a charge which is drawn towards the liquid crystal by the electric field. This makes the liquid crystal transparent at those locations. The overall pattern of transparency and opacity can be read off the liquid crystal layer using a light-based digital scanner and presented as a digital image. This research is of significance because of the fact that it separates the read-out system from the X-ray mechanism.
As pulmonary tuberculosis is becoming an epidemic in the developing countries, development of this technique is a boon to the people.
When I was working for my Ph.D., my guide (Dr. Shankar C. Bennur (now retired) Professor of Organic Chemistry, Karnatak University Dharwad, Karnatak, India) used to tell me that the liquid crystals will have many fold uses in the days to come. He did work (UFSC, Florianopolis, SC, Brazil) on the synthesis of many liquid crystals and used to tell me about his experience with this interesting field (which was at nascent stage). Whenever we used to get products (in my case, the compounds had methylene aminoxy methyl moiety) with low melting points, he used to elaborate about smectic point./long chain compounds.....Hope, he will be happy about this innovative idea. Congrats Dr.Rowland......
Ref : http://www.allbusiness.com/medicine-health/diseases-disorders-respiratory-disease/12124600-1.html
Subscribe to:
Posts (Atom)




