Ukoniq is the first and only, oral, once daily, inhibitor of phosphoinositide 3 kinase (PI3K) delta and casein kinase 1 (CK1) epsilon. Accelerated approval was granted for these indications based on overall response rate (ORR) data from the Phase 2 UNITY-NHL Trial (NCT02793583). Continued approval for these indications may be contingent upon verification and description of clinical benefit in a confirmatory trial. This application was granted priority review for the MZL indication. In addition, Ukoniq was granted Breakthrough Therapy Designation (BTD) for the treatment of MZL and orphan drug designation (ODD) for the treatment of MZL and FL.
Michael S. Weiss, Executive Chairman and Chief Executive Officer of TG Therapeutics stated, “Today’s approval of Ukoniq marks a historic day for our Company with this being our first approval and we are extremely pleased to be able to bring our novel inhibitor of PI3K-delta and CK1-epsilon to patients with relapsed/refractory MZL and FL. We have built a commercial team with significant experience who will immediately start to engage our customers to educate them on Ukoniq and how to access the product for patients in need and expect to make Ukoniq available to US distributors in the next few days.” Mr. Weiss continued, “We want to thank the patients, physicians, nurses and clinical coordinators for their support and participation in our clinical trials, and the FDA for their collaboration throughout this process. We remain dedicated to patients with B-cell diseases and our mission of developing treatment options for those in need.”
“Despite treatment advances, MZL and FL remain incurable diseases with limited treatment options for patients who relapse after prior therapy and no defined standard of care. With the approval of umbralisib we now have a targeted, oral, once-daily option, offering a needed treatment alternative for patients,” stated Dr. Nathan Fowler, Professor of Medicine at The University of Texas MD Anderson Cancer Center and the Study Chair of the UNITY-NHL MZL &FL cohorts.
“The approval of umbralisib for the treatment of relapsed/refractory marginal zone lymphoma and follicular lymphoma offers patients a new treatment option, and new hope in the fight against these diseases,” stated Meghan Gutierrez, Chief Executive Officer of the Lymphoma Research Foundation.
The safety of Ukoniq monotherapy was based on a pooled population from the 221 adults with MZL and FL in three single arm, open label trials and one open label extension trial. Patients received Ukoniq 800 mg orally once daily. Serious adverse reactions occurred in 18% of patients who received Ukoniq. Serious adverse reactions that occurred in ≥2% of patients were diarrhea-colitis (4%), pneumonia (3%), sepsis (2%), and urinary tract infection (2%). The most common adverse reactions (>15%), including laboratory abnormalities, were increased creatinine (79%), diarrhea-colitis (58%, 2%), fatigue (41%), nausea (38%), neutropenia (33%), ALT increase (33%), AST increase (32%), musculoskeletal pain (27%), anemia (27%), thrombocytopenia (26%), upper respiratory tract infection (21%), vomiting (21%), abdominal pain (19%), decreased appetite (19%), and rash (18%).


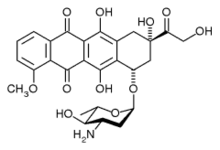 epirubicin
epirubicin
.png)



