Tuesday, December 6, 2011
UMass Amherst Researchers Test a Drug-Exercise Program Designed to Prevent Type 2 Diabetes
Monday, March 4, 2024
FDA Approves Brenzavvy (bexagliflozin) for the Treatment of Adults with Type 2 Diabetes
The FDA approval is based on results from a clinical program that evaluated the safety and efficacy of Brenzavvy in 23 clinical trials enrolling more than 5,000 adults with type 2 diabetes mellitus. Phase 3 studies showed Brenzavvy significantly reduced hemoglobin A1c and fasting blood sugar after 24 weeks, either as a monotherapy, in combination with metformin, or as an add-on to standard-of-care treatment consisting of a variety of regimens, including metformin, sulfonylureas, insulin, DPP4 inhibitors, or combinations of these agents. Although Brenzavvy is not approved for weight or blood pressure reduction, modest decreases in both weight and systolic blood pressure have been observed in the clinical program.
“As a class of drugs, SGLT2 inhibitors have shown tremendous benefit in treating adults with type 2 diabetes,” said Dr. Mason Freeman, M.D., Director of the Translational Research Center at Massachusetts General Hospital. “Being involved in all of the clinical trials for Brenzavvy, I am greatly impressed with the efficacy of the drug in reducing blood glucose levels and I believe it is an important addition to the SGLT2 inhibitor class of drugs.”
Brenzavvy treatment can be initiated in adults with type 2 diabetes with an estimated glomerular filtration rate (eGFR) greater than 30 mL/min/1.73 m2. Patients with eGFR less than 60 and greater than 30 mL/min/1.73 m2 are said to be in stage 3 chronic kidney disease, and for these patients metformin is often avoided due to the risk of lactic acidosis.
“Today's FDA approval represents a significant milestone for TheracosBio and provides an important treatment option to patients who suffer from type 2 diabetes. We look forward to bringing Brenzavvy to market,” said Albert R. Collinson, Ph.D., President and CEO of TheracosBio. “The approval of the Brenzavvy NDA is a result of the tireless work of the TheracosBio team and investigators. I want to thank all of the patients who took part in our clinical trials.”
According to the U.S. Centers for Disease Control and Prevention, more than 33 million Americans have type 2 diabetes, which means their bodies don’t use insulin correctly and as a result their blood sugar levels are too high. While some people can control their blood sugar levels with exercise and a healthy diet, others may need additional help to achieve good blood sugar (glycemic) control.
SGLT2 inhibitors are a class of prescription medicines that lower blood sugar by causing the kidneys to remove sugar from the body through urine.
Brenzavvy is available as 20 mg oral tablets recommended to be taken once daily, in the morning with or without food.
Sunday, October 4, 2009
Combination of Depagliflozin & Metaformin for type 2 diabatic ?

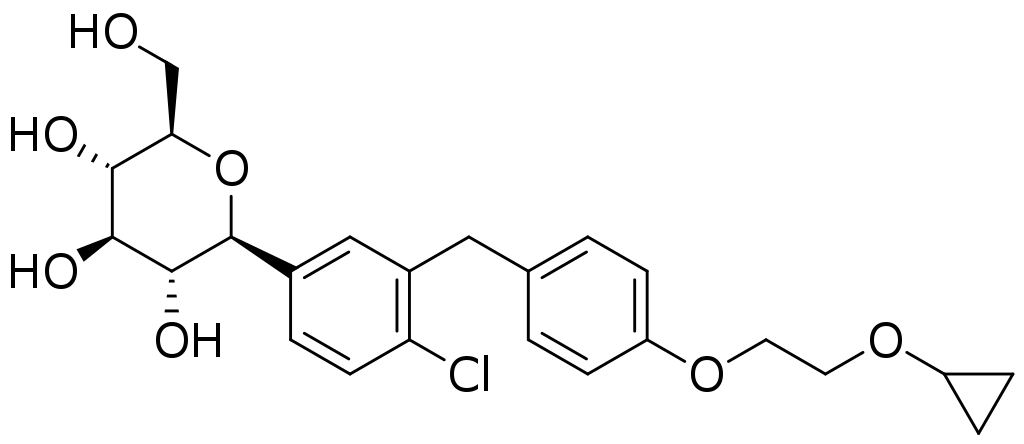
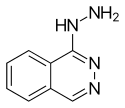
 We knew that these two Depagliflozin (left) & Metaformin (right) compounds were being studied independently for type 2 diabetic condition. Dapagliflozin, an investigational compound, is a potential first-in-class SGLT2 inhibitor currently in Phase 3 trials under joint development as a once-daily oral therapy for the treatment of type 2 diabetes. SGLT2 inhibitors facilitate the elimination of glucose by the kidney, thereby returning serum glucose levels towards normal.
We knew that these two Depagliflozin (left) & Metaformin (right) compounds were being studied independently for type 2 diabetic condition. Dapagliflozin, an investigational compound, is a potential first-in-class SGLT2 inhibitor currently in Phase 3 trials under joint development as a once-daily oral therapy for the treatment of type 2 diabetes. SGLT2 inhibitors facilitate the elimination of glucose by the kidney, thereby returning serum glucose levels towards normal.A recent study (24-week phase 3 clinical study by Bristol-Myers Squibb Company and AstraZeneca) demonstrated that the investigational drug dapagliflozin, added to metformin, demonstrated significant mean reductions in the primary endpoint, glycosylated hemoglobin level (HbA1c) and in the secondary endpoint, fasting plasma glucose (FPG) in patients with type 2 diabetes inadequately controlled with metformin alone, as compared to placebo plus metformin. Dapagliflozin is a novel, selective, sodium glucose co-transporter 2 (SGLT2) inhibitor.
The study also showed that individuals receiving dapagliflozin had statistically greater mean reductions in body weight compared to individuals taking placebo. Results from the 24-week study were presented at the 45th European Association for the Study of Diabetes Annual Meeting. This is the first public presentation of dapagliflozin Phase 3 data.
More interestingly, data on weight loss and blood pressure may be important adjuvants to glycemic control and is of great importance and hope in the days to come the SGLT2 inhibitors ( improved glycemic control) will play an important role in the type 2 diabetes. Given the continued rising prevalence of type 2 diabetes, there is an urgent need to have drugs of this kind..
Ref : http://www.astrazeneca.com/media/latest-press-releases/Dapagliflozen_Study014_EASD?itemId=7108139
Saturday, September 25, 2010
Saturday, August 18, 2012
Dapagliflozin more effective than sitagliptin for adult patients with type 2 diabetes
"Type 2 diabetes is a complex disease that often requires patients to take multiple treatments to control their blood sugar levels, with DPP4 inhibitors being some of the most widely prescribed therapies," said Serge Jabbour, M.D., Division Director of Endocrinology, Thomas Jefferson University. "In this study, dapagliflozin, in addition to diet and exercise, resulted in reduced blood sugar levels when added to sitagliptin, a DPP4 inhibitor. These findings add to our understanding of the effect of dapagliflozin in combination with commonly prescribed type 2 diabetes treatments."
Tuesday, September 20, 2011
Saturday, May 31, 2014
Combination of metformin and rapamycin shows potential in treating aging and related diseases
Monday, June 11, 2012
Lilly, Boehringer Ingelheim announce results from linagliptin Phase III trial on T2D
Wednesday, February 11, 2015
Diabetes drug can boost efficacy of TB medication without causing drug resistance
Friday, May 18, 2012
Two-Drug Therapy Helped Kids With Type 2 Diabetes
Thursday, June 16, 2022
FDA Approves Mounjaro (tirzepatide) Injection for the Treatment of Adults with Type 2 Diabetes
The U.S. Food and Drug Administration (FDA) has approved Mounjaro (tirzepatide) injection, Eli Lilly and Company's (NYSE: LLY) new once-weekly GIP (glucose-dependent insulinotropic polypeptide) and GLP-1 (glucagon-like peptide-1) receptor agonist indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes. Mounjaro has not been studied in patients with a history of pancreatitis and is not indicated for use in patients with type 1 diabetes mellitus.
As the first and only FDA-approved GIP and GLP-1 receptor agonist, Mounjaro is a single molecule that activates the body's receptors for GIP and GLP-1, which are natural incretin hormones.1
"Mounjaro delivered superior and consistent A1C reductions against all of the comparators throughout the SURPASS program, which was designed to assess Mounjaro's efficacy and safety in a broad range of adults with type 2 diabetes who could be treated in clinical practice. The approval of Mounjaro is an exciting step forward for people living with type 2 diabetes given the results seen in these clinical trials," said Juan Pablo Frías, M.D., Medical Director, National Research Institute and Investigator in the SURPASS program.
Mounjaro will be available in six doses (2.5 mg, 5 mg, 7.5 mg, 10 mg, 12.5 mg, 15 mg) and will come in Lilly's well-established auto-injector pen with a pre-attached, hidden needle that patients do not need to handle or see.
The approval was based on results from the phase 3 SURPASS program, which included active comparators of injectable semaglutide 1 mg, insulin glargine and insulin degludec. Efficacy was evaluated for Mounjaro 5 mg, 10 mg and 15 mg used alone or in combination with commonly prescribed diabetes medications, including metformin, SGLT2 inhibitors, sulfonylureas and insulin glargine. Participants in the SURPASS program achieved average A1C reductions between 1.8% and 2.1% for Mounjaro 5 mg and between 1.7% and 2.4% for both Mounjaro 10 mg and Mounjaro 15 mg. While not indicated for weight loss, mean change in body weight was a key secondary endpoint in all SURPASS studies. Participants treated with Mounjaro lost between 12 lb. (5 mg) and 25 lb. (15 mg) on average.1
Side effects reported in at least 5% of patients treated with Mounjaro include nausea, diarrhea, decreased appetite, vomiting, constipation, indigestion (dyspepsia), and stomach (abdominal) pain. The labeling for Mounjaro contains a Boxed Warning regarding thyroid C-cell tumors. Mounjaro is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or in patients with Multiple Endocrine Neoplasia syndrome type 2.1
"Lilly has a nearly 100-year heritage of advancing care for people living with diabetes – never settling for current outcomes. We're not satisfied knowing that half of the more than 30 million Americans living with type 2 diabetes are not reaching their target blood glucose levels," said Mike Mason, president, Lilly Diabetes. "We are thrilled to introduce Mounjaro, which represents the first new class of type 2 diabetes medication introduced in almost a decade and embodies our mission to bring innovative new therapies to the diabetes community."
Tuesday, October 30, 2012
Dulaglutide Fares Well in New Trials
Monday, June 9, 2014
Isis Pharmaceuticals reports positive data from ISIS-GCGRRx Phase 2 study in patients with type 2 diabetes
Thursday, October 10, 2019
FDA Approves Victoza (liraglutide) for the Treatment of Pediatric Patients 10 Years or Older with Type 2 Diabetes
“The FDA encourages drugs to be made available to the widest number of patients possible when there is evidence of safety and efficacy,” said Lisa Yanoff, M.D, acting director of the Division of Metabolism and Endocrinology Products in the FDA’s Center for Drug Evaluation and Research. “Victoza has now been shown to improve blood sugar control in pediatric patients with type 2 diabetes. The expanded indication provides an additional treatment option at a time when an increasing number of children are being diagnosed with this disease.”
Thursday, November 9, 2017
FDA Approves Once-Weekly Bydureon BCise (exenatide) for Patients with Type-2 Diabetes

In continuation of my update on exenatide. AstraZeneca announced that the US Food and Drug Administration (FDA) has approved Bydureon® BCise™ (exenatide extended-release) injectable suspension, a new formulation of Bydureon (exenatide extended-release) injectable suspension in an improved once-weekly, single-dose autoinjector device for adults with type-2 diabeteswhose blood sugar remains uncontrolled on one or more oral medicines inaddition to diet and exercise, to improve glycemic control.
Friday, March 3, 2017
This Diabetes Drug Saves Lives. You Can Thank The FDA
Friday, June 3, 2011
Lyxumia®, as an add-on to basal Insulin, shows significant positive phase III results
Monday, January 29, 2018
FDA-approved drug to treat high blood pressure increases life span in worms
"This is the first report of hydralazine treatment activating the NRF2/SKN-1 signaling pathway. We found the drug extends the life span of worms as well as or better than other potential anti-aging compounds such as curcumin and metformin. The treatment also appeared to maintain their health as measured by tests of flexibility and wiggling speed," said Dr. Hamid Mirzaei, Assistant Professor of Biochemistry at UT Southwestern and senior author of the study, published today in Nature Communications.
"Age-related neurodegenerative diseases are devastating, and those conditions are on the rise due to the increase in the life span of humans. For that reason, it is important to develop treatments to maintain human health as long as possible," said Dr. Mirzaei, who is also an investigator in the Center for Alzheimer's and Neurodegenerative Diseases, part of the Peter O'Donnell Jr. Brain Institute at UT Southwestern.http://www.utsouthwestern.edu/newsroom/articles/year-2017/hbp-drug.html
Wednesday, April 7, 2021
Acid reflux drug may be a promising therapy to reduce preterm birth

Finding progesterone on the list was a promising validating step. Four of the drugs on our list have seen effectiveness in past studies that were either experimental or retrospective. This leads us to believe in the biology behind the identification of these drugs."Brian Le, PhD, postdoctoral scholar in the UCSF Department of Pediatrics and the Bakar Computational Health Sciences Institute, and the first author of the study