Monday, October 17, 2016
Diabetes drug found no better than placebo at treating nonalcoholic fatty liver disease: But randomized, double-blind clinical trial suggests better way to conduct future trials
Saturday, January 30, 2021
Sitagliptin Promising Addition for Preventing Acute GVHD
For patients undergoing myeloablative allogeneic hematopoietic stem cell transplantation, sitagliptin combined with tacrolimus and sirolimus results in a low incidence of grade II to IV acute graft-versus-host disease (GVHD) by day 100, according to a study published in the Jan. 7 issue of the New England Journal of Medicine.
Sherif S. Farag, M.D., Ph.D., from the Indiana University School of Medicine in Indianapolis, and colleagues conducted a phase 2 clinical trial to examine the reduction in incidence of grade II to IV acute GVHD from 30 percent to no more than 15 percent by day 100 with sitagliptin plus tacrolimus and sirolimus. Thirty-six patients received myeloablative conditioning followed by mobilized peripheral-blood stem cell transplants from matched related or unrelated donors.
The researchers found that by day 100, acute GVHD occurred in two of 36 patients. The incidence of grade II to IV GVHD and of grade III or IV GVHD was 5 and 3 percent, respectively. At one year, nonrelapse mortality was zero. The one-year cumulative incidence of relapse was 26 percent, and for chronic GVHD, it was 37 percent. At one year, GVHD-free, relapse-free survival was 46 percent. Toxic effects were similar to those seen in patients undergoing allogeneic stem cell transplantation.
"Inhibition of dipeptidyl peptidase 4 should be further investigated in randomized trials that compare sitagliptin with current standard GVHD prophylaxis regimens," the authors write.
https://en.wikipedia.org/wiki/Sitagliptin
Saturday, August 18, 2012
Dapagliflozin more effective than sitagliptin for adult patients with type 2 diabetes
"Type 2 diabetes is a complex disease that often requires patients to take multiple treatments to control their blood sugar levels, with DPP4 inhibitors being some of the most widely prescribed therapies," said Serge Jabbour, M.D., Division Director of Endocrinology, Thomas Jefferson University. "In this study, dapagliflozin, in addition to diet and exercise, resulted in reduced blood sugar levels when added to sitagliptin, a DPP4 inhibitor. These findings add to our understanding of the effect of dapagliflozin in combination with commonly prescribed type 2 diabetes treatments."
Saturday, February 4, 2012
FDA Approves Jentaduet ((sitagliptin and metformin hydrochloride (HCl) )...
Monday, October 10, 2011
First combination drug to treat type 2 diabetes and high cholesterol receives FDA approval
Tuesday, October 30, 2012
Dulaglutide Fares Well in New Trials
Tuesday, December 6, 2016
FDA Expands Indication of Invokamet (canagliflozin/metformin HCl) to Include First-Line Treatment of Type 2 Diabetes
 metformin
metformin 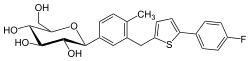 canagliflozin
canagliflozinPhase 3 Study Supports Expanded Indication
Other Phase 3 Studies of Canagliflozin-Metformin Therapy
About Type 2 Diabetes
Saturday, July 14, 2018
Semaglutide found to be effective against type 2 diabetes

Semaglutide is safe and effective for the treatment of type 2 diabetes, according to a review published online May 13 in Diabetes, Obesity and Metabolism.
"Semaglutide is a potent once-weekly glucagon-like peptide 1 receptor agonist, reducing significantly HbA1c, body weight, and systolic blood pressure. However, it is associated with increased incidence of gastrointestinal adverse events," the authors write.
Friday, March 20, 2020
FDA Approves Rybelsus (semaglutide), the First Oral GLP-1 Analog Treatment for Adults with Type 2 Diabetes

In continuation of my updates on Semaglutide
"GLP-1 receptor agonists are effective medications for people with type 2 diabetes but have been underutilized in part because they have, until now, only been available as an injectable treatment," said Vanita R. Aroda, MD, Director of Diabetes Clinical Research, Brigham and Women's Hospital, Boston, MA and a PIONEER clinical trial investigator. "The availability of an oral GLP-1 receptor agonist represents a significant development and primary care providers, specialists and patients alike may now be more receptive to the use of a GLP-1 therapy to help them achieve their blood sugar goals."
"People living with type 2 diabetes deserve more innovation, research and support to help them achieve their individual A1C goals," said Todd Hobbs, vice president and U.S. chief medical officer of Novo Nordisk. "With Rybelsus, we have the opportunity to expand use of effective GLP-1 receptor agonist therapy by providing adults with type 2 diabetes an oral medication which was previously only available as an injection to help with managing their blood sugar."



