Blueprint Medicines Corporation (NASDAQ: BPMC), a precision therapy company focused on genomically defined cancers, rare diseases and cancer immunotherapy, today announced that the U.S. Food and Drug Administration (FDA) has accepted the company's New Drug Application (NDA) for avapritinib for the treatment of adult patients with PDGFRA Exon 18 mutant gastrointestinal stromal tumors (GIST), regardless of prior therapy, and fourth-line GIST. The FDA granted Priority Review and set an action date of February 14, 2020 under the Prescription Drug User Fee Act (PDUFA). At this time, the FDA is not planning to hold an advisory committee meeting to discuss this application. Avapritinib, an investigational therapy, is a potent and highly selective KIT and PDGFRA inhibitor for patients with advanced GIST.
"Patients with PDGFRA Exon 18 mutant GIST and fourth-line GIST are in need of new treatment options that address the underlying drivers of the disease," said Andy Boral, M.D., Ph.D., Chief Medical Officer at Blueprint Medicines. "The FDA's acceptance of our application for Priority Review brings us closer to our goal of delivering avapritinib to patients with GIST, and we look forward to working closely with the FDAduring the review process."
The FDA's acceptance of the NDA indicates the application is sufficiently complete to permit a substantive review. A Priority Review designation accelerates the FDA's review time from 12 months to a goal of eight months from the NDA submission date, and is granted to drugs that may offer a significant improvement in the safety or effectiveness of the treatment, prevention or diagnosis of a serious condition. Previously, the FDA granted avapritinib Breakthrough Therapy Designation for the treatment of patients with unresectable or metastatic GIST harboring the PDGFRα D842V mutation.
In July 2019, the European Medicines Agency validated Blueprint Medicines' Marketing Authorization Application for avapritinib in adult patients with PDGFRα D842V mutant GIST, regardless of prior therapy, and fourth-line GIST.
About GIST
GIST is a sarcoma, or tumor of bone or connective tissue, of the gastrointestinal (GI) tract. Tumors arise from cells in the wall of the GI tract and occur most often in the stomach or small intestine. Most patients are diagnosed between the ages of 50 to 80, and diagnosis is typically triggered by GI bleeding, incidental findings during surgery or imaging and, in rare cases, tumor rupture or GI obstruction.
Most GIST cases are caused by a spectrum of clinically relevant mutations that force the KIT or PDGFRA protein kinases into an increasingly active state. Because currently available therapies primarily bind to the inactive protein conformations, certain primary and secondary mutations typically lead to treatment resistance and disease progression.
In unresectable or metastatic GIST, clinical benefits from existing treatments can vary by mutation type. Mutational testing is critical to tailor therapy to the underlying disease driver and is recommended in expert guidelines. Currently, there are no approved therapies for patients with KIT-driven GIST whose disease progresses beyond imatinib, sunitinib and regorafenib. In patients with metastatic PDGFRα D842V-driven GIST, progression occurs in a median of approximately three to four months with available therapy.
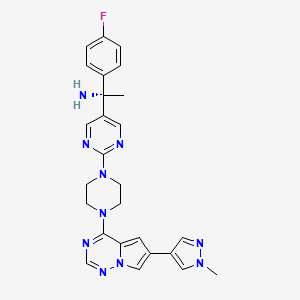
https://pubchem.ncbi.nlm.nih.gov/compound/Avapritinib#section=2D-Structure