Genentech, a member of the Roche Group (SIX: RO, ROG; OTCQX: RHHBY), announced the U.S. Food and Drug Administration (FDA) has approval of Rozlytrek (entrectinib) for the treatment of adults with ROS1-positive, metastatic non-small cell lung cancer (NSCLC). The FDA has also granted accelerated approval to Rozlytrek for the treatment of adult and pediatric patients 12 years of age and older with solid tumors that have a neurotrophic tyrosine receptor kinase (NTRK) gene fusion without a known acquired resistance mutation, are metastatic or where surgical resection is likely to result in severe morbidity, and have progressed following treatment or have no satisfactory alternative therapy.
These approvals are based on results from the integrated analysis of the pivotal Phase II STARTRK-2, Phase I STARTRK-1 and Phase I ALKA-372-001 trials, and data from the Phase I/II STARTRK-NG study. In the integrated analysis, Rozlytrek was studied in several solid tumor types, including breast, cholangiocarcinoma, colorectal, gynecological, neuroendocrine, non-small cell lung, salivary gland, pancreatic, sarcoma and thyroid cancers. In ROS1-positive, metastatic NSCLC, Rozlytrek shrank tumors in 78% of people with the disease (overall response rate [ORR]; N=51) and the duration of response (DoR) ranged from 1.8 to 36.8+ months (N=40 out of 51). Rozlytrek also shrank tumors in more than half of people with NTRK gene fusion-positive, locally advanced or metastatic solid tumors (ORR=57%; N=54), and objective responses were observed across 10 tumor types (DoR ranged from 2.8 to 26.0+ months; N=31 out of 54). Objective responses to Rozlytrek were seen in people with central nervous system (CNS) metastases at baseline.
“Rozlytrek’s FDA approval for two rare types of cancer is an important advance for patients, combining a targeted medicine and genomic testing to bring this new treatment option to patients who are waiting,” said Sandra Horning, M.D., chief medical officer and head of Global Product Development. “Rozlytrek is the first FDA-approved treatment that selectively targets both ROS1 and NTRK fusions, and, importantly, has also shown responses in these rare cancer types that have spread to the brain.”
“The identification of actionable biomarkers like ROS1 has brought about significant progress in the treatment of lung cancer. This approval brings further hope to people with this rare type of the disease,” said Janet Freeman-Daily, co-founder of The ROS1ders, a group of patients and caregivers affected by ROS1-positive lung cancer. “Up to 40% of people with ROS1-positive non-small cell lung cancer have tumors that have spread to the brain, so now there is a new treatment option for those patients.”
The most common adverse reactions (≥20 percent) with Rozlytrek were fatigue, constipation, altered sense of taste (dysgeusia), swelling (edema), dizziness, diarrhea, nausea, nervous system disorders (dysesthesia), shortness of breath (dyspnea), muscle pain (myalgia), cognitive impairment, increased weight, cough, vomiting, fever (pyrexia), joint pain (arthralgia) and vision disorders.
The FDA’s Accelerated Approval Program allows conditional approval of a medicine that fills an unmet medical need for a serious or life-threatening disease or condition. The accelerated approval of Rozlytrek for NTRK gene fusion-positive solid tumors is based on tumor response rate and durability of response, and continued approval may be contingent upon verification and description of clinical benefit in the confirmatory trials.
Biomarker testing for ROS1 in NSCLC and NTRK gene fusions across all solid tumors is the only way to identify people who are eligible for treatment with Rozlytrek. Genentech is leveraging its expertise in developing personalized medicines and advanced diagnostics, in conjunction with Foundation Medicine, to help identify people with ROS1 and NTRK gene fusions. Foundation Medicine will submit Foundation®One CDx to the FDA for approval as a companion diagnostic for Rozlytrek. An FDA-approved companion diagnostic for Rozlytrek is not available at this time.
Rozlytrek is now available in the United States for adults and children 12 years of age and older. For those who qualify, Genentech offers patient assistance programs for people prescribed Rozlytrek by their doctor through Genentech Access Solutions. Please contact Genentech Access Solutions at (866) 422-2377 or visit http://www.Genentech-Access.comfor more information.
About the Integrated Analysis
This approval is based on an integrated analysis including data from 51 people with ROS1-positive NSCLC and 54 people with locally advanced or metastatic NTRK gene fusion-positive solid tumors (10 tumor types, >19 histopathologies) from the Phase II STARTRK-2, Phase I STARTRK-1 and Phase I ALKA-372-001 trials. This approval is also based on data from the Phase I/II STARTRK-NG study in pediatric patients. The studies enrolled people across 15 countries and more than 150 clinical trial sites. Safety was assessed from an integrated analysis of 355 people across these four trials.
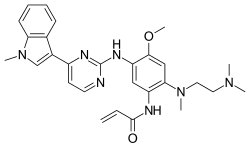
https://en.wikipedia.org/wiki/Entrectinib
https://pubchem.ncbi.nlm.nih.gov/compound/Entrectinib#section=2D-Structure

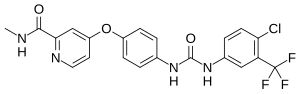
 Crizotinib
Crizotinib