Friday, January 22, 2016
Helsinn one step closer to bringing anamorelin HCI to market for treatment of anorexia, cachexia in NSCLC patients
Tuesday, December 10, 2013
Toxicity limits benefits of bevacizumab–erlotinib NSCLC maintenance therapy
Wednesday, August 7, 2013
FDA Approves Gilotrif for Late Stage Non-Small Cell Lung Cancer
“Today’s approvals further illustrate how a greater understanding of the underlying molecular pathways of a disease can lead to the development of targeted treatments,” said Richard Pazdur, M.D., director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “Gilotrif is the second drug approved this year for patients with untreated metastatic NSCLC whose tumors have the EGFR exon 19 deletions or exon 21 L858R substitution mutations.”
Thursday, October 18, 2012
Synta announces results from ganetespib Phase 2b trial on NSCLC
"The preliminary results from GALAXY indicate that the addition of ganetespib to docetaxel is well tolerated and may improve outcomes in patients compared to docetaxel alone," said Dr. Ramalingam, a Principal Investigator of the study. "This includes promising improvements in survival seen across the broad adenocarcinoma population as well as in key predefined patient populations. A well-tolerated combination regimen that extends survival associated with salvage therapy in NSCLC will meet a much awaited need to improve the current standard of care."
Tuesday, November 5, 2013
Metformin could serve as radiosensitizer to treat patients with stage III non-small cell lung cancer
Friday, January 9, 2015
New targeted therapy shows promise in patients with ALK-positive advanced NSCLC
Wednesday, November 20, 2013
Nintedanib drug to treat NSCLC is submitted for approval from European Medicines Agency
Thursday, June 2, 2016
Xalkori Approved For Rare Genetic Form of Lung Cancer
Tuesday, November 4, 2014
Friday, December 24, 2010
Thursday, April 9, 2015
LUME-Lung 1 shows QoL, symptoms benefits
Saturday, June 13, 2009
Cisplatin doubles lung cancer survival time in mice !
After so many years, I could find this something interesting findings about cisplatin, by Patrizia Russo of Lung Cancer Unit of the National Cancer Research Institute in Genoa, Italy and colleagues from San Raffaele Pisana Scientific Institute for Research, Hospitalization and Health Care (IRCCS), Catholic University.
In the study, the authors took the research a step further and showed that α-CbT could inhibit non-small cell lung carcinoma (NSCLC) growth and prolong life in non-obese/severe combined immunodeficient (NOD/SCID) mice that had human NSCLC grafted to their lungs. This study attempted to mimic human cancer conditions more closely by delaying treatment until the tumors were well-established. In addition to control mice that were untreated, the researchers randomized one third of the mice to receive standard chemotherapy.
They found that NOD/SCID mice treated with the standard chemotherapy agent, cisplatin, had a 16 percent longer median survival time than untreated mice (p= 0.05). Mice treated with α-CbT, however, had an increased median survival time of 1.7-fold over the cisplatin-treated mice and 2.1-fold over the no-treatment controls (p=0.0005). Though the clinical trials to establish the claim and to to explore the widest range of possibilities of intervention on the α7-nAChRs. Congrats...
Ref :Inhibition of Nonneuronal 7-Nicotinic Receptor for Lung Cancer Treatment; Am. J. Respir. Crit. Care Med., Jun 2009; 179: 1141 - 1150
Monday, July 30, 2012
Drug Combo Tackling Solid Tumors
“There is progress being made in the treatment of lung cancer but survival rates still remain low. This is because the majority of patients – up to two thirds – are diagnosed once the cancer has already spread to other organs when it’s more difficult to treat successfully.
“We hope that this new approach may eventually contribute to increased survival for lung cancer patients.”
Ref : http://cancerhelp.cancerresearchuk.org/trials/a-trial-of-vandetanib-and-selumetinib-for-solid-tumours-including-nsclc-vansel-1
Thursday, March 24, 2016
Afatinib a better choice for EGFR-mutated lung cancer in first-line treatment
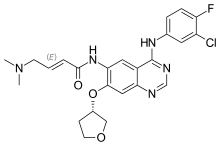
In continuation of my update on Afatinib
Thursday, December 10, 2015
Early trial results in lung cancer

Results from early phase trials investigating different therapeutic agents in lung cancer patients were presented during the third Presidential Session at the European Cancer Congress in Vienna, Austria. Here we summarise two studies reported at the session.
Monday, November 29, 2010
PARP inhibitor, MK-4827, shows anti-tumour activity in first trial in humans....
Monday, February 18, 2013
Breakthrough in ovarian cancer: Selumetinib
"There just aren't very good treatments for low-grade ovarian cancer, so this discovery opens up a lot of new exciting possibilities for us," Dr. Farley said. He added that Phase III of this trial is scheduled to begin in the next few weeks, with that trial to be the "definitive test" before the treatment becomes available to the general population.
Breakthrough in ovarian cancer: Selumetinib
Thursday, September 3, 2015
Brigatinib drug shows promise against ALK non-small cell lung cancer in phase I/II clinical trial
Friday, December 17, 2021
New Drug Application of Plinabulin (Response Letter from the FDA) for Prevention of Chemotherapy-Induced Neutropenia (CIN)...
BeyondSpring Pharmaceuticals announced the receipt of a Complete Response Letter (CRL) from the U.S. Food and Drug Administration (FDA) for the New Drug Application (NDA) seeking approval of plinabulin in combination with granulocyte colony-stimulating factor (G-CSF) for the prevention of chemotherapy-induced neutropenia (CIN). The FDA issued the CRL to indicate that they have completed their review of the application and have determined that it cannot be approved in its present form.
The FDA’s CRL indicated that the results of the single registrational trial (106 Phase 3) was not sufficiently robust to demonstrate benefit and that a second well controlled trial would be required to satisfy the substantial evidence requirement to support the CIN indication.
“BeyondSpring strongly believes that plinabulin in combination with G-CSF has significant potential to raise the standard of care in CIN, a devastating side effect of chemotherapy,” said Dr. Lan Huang, BeyondSpring’s co-founder, chief executive officer and chairwoman. “The Company plans to request a meeting with the FDA and remains committed to its goal of bringing plinabulin to cancer patients in need globally.”
BeyondSpring remains confident in the efficacy and safety data for plinabulin in combination with G-CSF for the prevention of CIN. The Company expects to work closely with the FDA to consider the possible future clinical pathway for CIN, which may include a second study.
Plinabulin is the first drug candidate submitted for FDA approval that has the potential to work in the critical first week of chemotherapy treatment before G-CSF is effective, to prevent the onset and improve clinical outcomes of CIN.
Plinabulin, BeyondSpring’s lead asset, is a selective immunomodulating microtubule-binding agent (SIMBA), which is a potent antigen presenting cell (APC) inducer. It is a novel, intravenous infused, patent-protected, NDA-stage asset for CIN prevention and a Phase 3 anti-cancer candidate for non-small cell lung cancer (NSCLC) with recently released positive topline data. Plinabulin triggers the release of the immune defense protein, GEF-H1, which leads to two distinct effects: first is a durable anticancer benefit due to the maturation of dendritic cells resulting in the activation of tumor antigen-specific T-cells to target cancer cells, and the second is early-onset of action in CIN prevention after chemotherapy by boosting the number of hematopoietic stem/progenitor cells (HSPCs). Plinabulin received Breakthrough Therapy designation and priority review from both U.S. and China FDA for the CIN prevention indication. As a “pipeline in a drug,” plinabulin is being broadly studied in combination with various immuno-oncology agents that could boost the effects of the PD-1/PD-L1 antibodies and re-sensitize PD-1/PD-L1 antibody-resistant patients.
https://en.wikipedia.org/wiki/Plinabulin
Thursday, January 27, 2022
Spectrum Pharmaceuticals Submits New Drug Application for Poziotinib
Spectrum Pharmaceuticals, a biopharmaceutical company focused on novel and targeted oncology therapies, announced the submission of its New Drug Application (NDA) for poziotinib to the U.S. Food and Drug Administration (FDA) for use in patients with previously treated locally advanced or metastatic non-small cell lung cancer (NSCLC) with HER2 exon 20 insertion mutations. The NDA submission is based on the positive results of Cohort 2 from the ZENITH20 clinical trial, which assessed the safety and efficacy of poziotinib. The product has received Fast Track designation and there is currently no treatment specifically approved by the FDA for this indication.
“The NDA submission for poziotinib marks an important step in achieving a first treatment for patients with HER2 exon 20 insertion mutations in lung cancer,” said Joe Turgeon, President and CEO of Spectrum Pharmaceuticals. “I want to thank the patients, investigators and our internal staff who have passionately worked to achieve this important milestone in an area of high unmet medical need.”
ZENITH20 Cohort 2 Clinical Results Summary
Results for Cohort 2 of the ZENITH20 clinical trial have been published in the Journal of Clinical Oncology (November 29, 2021), and can be accessed by clicking here.
Cohort 2 enrolled 90 patients who received an oral once daily dose of 16 mg of poziotinib. The intent-to-treat analysis demonstrated a confirmed objective response rate (ORR) of 27.8% (95% Confidence Interval (CI), 18.9%-38.2%). The observed lower bound of 18.9% exceeded the pre-specified lower bound of 17%. The median duration of response was 5.1 months and the median progression free survival was 5.5 months. In this cohort, 87% of patients had drug interruptions with 11 patients (12%) permanently discontinuing due to adverse events. 13 patients (14%) had treatment-related serious adverse events. As previously announced, the company had a successful pre-NDA meeting with the FDA which resulted in an agreement to submit an NDA for poziotinib. During the meeting, Spectrum confirmed with the FDA that Cohort 2 data could serve as the basis of an NDA submission. The company will continue to work with the FDA as appropriate, while the agency conducts its review.
More : https://investor.sppirx.com/news-releases/news-release-details/spectrum-pharmaceuticals-submits-new-drug-application-poziotinib
https://en.wikipedia.org/wiki/Poziotinib










