Scientists at The Scripps Research Institute (TSRI) have devised a new molecule-building method that is likely to have a major impact on the pharmaceutical industry and many other chemistry-based enterprises.
The method, published as an online First Release paper in Science on April 21, 2016, allows chemists to construct novel, complex and potentially very valuable molecules, starting from a large class of compounds known as carboxylic acids, which are relatively cheap and non-toxic. Carboxylic acids include the amino acids that make proteins, fatty acids found in animals and plants, citric acid, acetic acid (vinegar) and many other substances that are already produced in industrial quantities.
"This is one of the most useful methods we have ever worked with, and it mostly involves materials that every chemist has access to already, so I think the interest in it will expand rapidly," said principal investigator Phil S. Baran, Darlene Shiley Professor of Chemistry at TSRI.
"This exciting new discovery represents a significant advance in our ability to transform simple organic molecules and to rapidly build complex structures from readily available materials—we expect to use it in both the discovery and development of biologically active compounds that help patients prevail over serious disease," said co-author Martin D. Eastgate, a Director in Chemical and Synthetic Development at Bristol-Myers Squibb, who participated in the study as part of a long-standing research collaboration between Bristol-Myers Squibb and TSRI.
The new method is a modification of what is already one of the most widely used sets of chemical reactions: amide bond-forming reactions. These occur naturally in cells to stitch together amino-acids into proteins, for example. Since the 1940s, when they became a popular tool for laboratory chemists, they have been instrumental in the discovery of many new compounds as well as new methods for synthesizing compounds.
Amide bond-forming reactions couple carbon atoms on carboxylic acids to nitrogen atoms on another broad class of compounds called amines. The reactions are relatively safe and easy, and produce water, H2O, as a co-product. Chemists have long dreamed of using similarly cheap and easy techniques to make carbon-to-carbon couplings. That would enable them to synthesize, and potentially turn into drugs and other useful products, an enormous number of organic molecules that have previously been inaccessible.
Carbon to Carbon
The method devised by Baran and his team essentially repurposes the traditional amide bond-forming strategy to achieve carbon-carbon couplings. The new reactions again involve easy, safe conditions—the co-product now is carbon dioxide, CO2—and the same inexpensive and widely available starting materials, carboxylic acids. This time the reaction partners are not nitrogen-containing amines but organic compounds containing carbon and zinc, which are also relatively easy to buy or make.
The path to the new invention began with a long-known reaction called the Barton decarboxylation. "We started by asking ourselves what would happen if we could use a metal to trap a radical [a highly reactive charged molecule] generated in the Barton decarboxylation," said TSRI Research Associate Josep Cornella. "We realized that if we could do that, it would open up a totally new approach to organic synthesis and carbon-carbon coupling."
The method the team ultimately developed employs an inexpensive and commercially available activating agent that primes the chosen carboxylic acid for the reaction. A metal catalyst—inexpensive nickel—then facilitates the reaction between the carboxylic acid and its carbon-zinc partner compound.
A key ingredient turned out to be a "ligand" compound that helps the metal catalyst do its job. "We found that common, readily available bipyridine ligands work best—these help to stabilize the nickel so it can catalyze the reaction," said TSRI Research Associate Tian Qin.

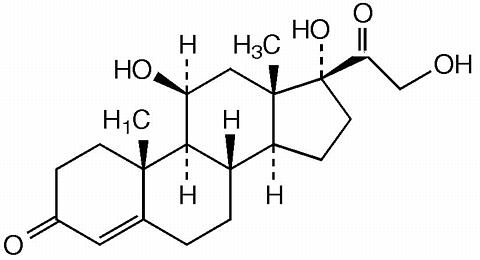



 Carfilzomib
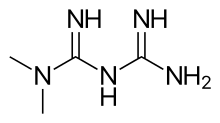
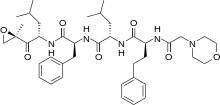
Carfilzomib 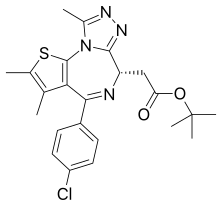 JQ1
JQ1  ABT-199
ABT-199