In continuation of my update on metformin
Researchers at the University of Cincinnati (UC) College of Medicine have found that adding increasing doses of an approved Type 2 diabetes drug, metformin, to a chemotherapy and radiation treatment regimen in head and neck cancer patients is not well tolerated if escalated too quickly, but allowing slower escalation could be beneficial.
These findings are being presented via poster June 4 at the 2016 American Society of Clinical Oncology (ASCO) Annual Meeting: Collective Wisdom, being held June 3-7 in Chicago.
Trisha Wise-Draper, MD, PhD, assistant professor in the Division of Hematology Oncology at the UC College of Medicine, a member of both the Cincinnati Cancer Center and UC Cancer Institute and principal investigator on this study, says retrospective studies have shown improved outcomes in tumors treated with chemotherapy and radiation if they were also on metformin for diabetes.
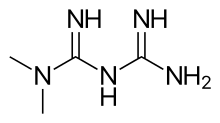
"In head and neck squamous cell carcinoma, which develops in the mucous membranes of the mouth, nose and throat, diabetic patients taking a medication called metformin had better overall survival compared to those not on metformin when also treated with chemotherapy and radiation," she says. "Additionally, pancreatic cancer patients treated with chemotherapy and metformin required higher doses of metformin--1,000 milligrams twice a day--to experience positive results.
"In basic science studies, metformin has been shown to stop mTOR, a molecular pathway present and active in this type of head and neck cancer, and pretreatment with metformin resulted in a decrease in the occurrence of oral cavity tumors in animal models. In this study, we wanted to see if the combination of escalating doses of metformin with the chemotherapy agent cisplatin and radiation for head and neck cancer tumors in non-diabetic patients would be effective."
Wise-Draper says that metformin, which is an approved Type 2 diabetes medication, was provided by their investigational pharmacy. Metformin was administered orally in escalating doses for 7 to 14 days prior to starting the cisplatin and radiation and continued throughout standard treatment. Blood samples were collected before and after metformin treatment as well as during chemotherapy. Flow cytometry, a technique used to count cells, was used to detect the percent of circulating immune activated cells, and clinical laboratory tests including glucose, B12 and C-peptide (an amino acid that is important for controlling insulin) were performed.
"This is part of an ongoing clinical trial," says Wise-Draper. "We found that eight patients with advanced head and neck cancer have been enrolled so far; we plan to have 30 total. Due to the relatively quick escalation of metformin, the patients' tolerance was poor with higher doses of metformin when initiated 7 days prior to their chemotherapy and radiation therapy regimen.
"Therefore, the protocol was modified to allow slower escalation over 14 days. The most common toxicities observed included nausea (71 percent of patients) and vomiting (43 percent of patients), increase in creatinine (57 percent of patients), decreased white blood cell count (43 percent of patients) and pain when swallowing (43 percent of patients) with only nausea being directly attributed to metformin and the rest attributed to cisplatin and radiation."
She adds that there wasn't a substantial change in T cell or glucose levels with administration of metformin in the small sample of patients but that there were increased C-peptide levels in response to metformin administration.
"These results show that the combination of metformin and cisplatin and radiation was poorly tolerated when metformin was escalated quickly. However, there has been no significant increase in side effects thus far with the addition of metformin," Wise-Draper says. "The trial is continuing with escalation of metformin over a longer period of time to provide more data; we will also try to increase our sample size."

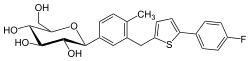




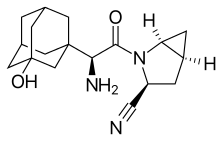 Saxagliptin and
Saxagliptin and