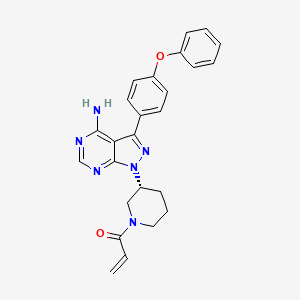
In continuation of my update on ibrutinib
New Cleveland Clinic research shows for the first time that ibrutinib, an FDA-approved drug for lymphoma and leukemia, may also help treat the most common—and deadliest—type of brain tumor. The findings, published in Science Translational Medicine, offer hope that the drug may one day be used in patients with glioblastoma and improve poor survival rates.
The team of researchers, led by Shideng Bao, Ph.D., of Cleveland Clinic's Lerner Research Institute found that ibrutinib slowed brain tumor growth in a preclinical model and extended survival more than 10-times the rate of the current standard-of-care chemotherapy drug.
They found in human glioblastoma cells that ibrutinib works by inhibiting glioma stem cells—an aggressive type of brain cancer cell that tends to resist treatment and spread. Furthermore, they showed that combining ibrutinib with radiation therapy prevents glioblastoma cells from developing this resistance. Combination therapy overcame resistance and extended lifespan more effectively than either radiation or ibrutinib treatment alone.
According to the American Brain Tumor Association, glioblastoma survival is very poor—median survival in patients undergoing standard treatment is less than 15 months.
"Glioblastoma is the most lethal primary brain tumor and is highly resistant to current therapies," said Bao. "There is an urgent need to get new treatments to these patients as quickly as possible."
In earlier studies, Bao and colleagues found that glioma stem cells have high levels of a protein called BMX (bone marrow and X-linked non-receptor tyrosine kinase). BMX activates a protein called STAT3 (signal transducer and activator of transcription 3), which is responsible for the aggressive, pro-cancer qualities of glioma stem cells. In this new study, the researchers found that ibrutinib works by inhibiting both proteins.
"Additional research is important to understand the effects of ibrutinib in patients, but these early findings are promising," said Bao. "Using an FDA-approved drug would allow us to surpass many of the lengthy regulatory studies needed when developing a new treatment, and we could potentially begin clinical trials very soon."
Ibrutinib (Imbruvica) has been approved by the U.S. Food & Drug Administration to treat certain types of leukemia and lymphoma, as well as chronic graft versus host disease.


