Capecitabine, is an orally-administered chemo therapeutic agent used in the treatment of
metastatic breast and colorectal cancers.
Mode of action :
Capecitabine is a prodrug, that is enzymatically converted to
5-fluorouracil in the tumor, where it inhibits DNA synthesis and slows growth of tumor tissue. The activation of capecitabine follows a pathway with three enzymatic steps and two intermediary metabolites, 5'-deoxy-5-fluorocytidine (5'-DFCR) and 5'-deoxy-5-fluorouridine (5'-DFUR), to form 5-fluorouracil. Its being used (& FDA approved) in the treatment of adjuvant in
colorectal cancer, metastatic colorectal cancer and
Metastatic breast cancer - used in combination with docetaxel, after failure of anthracycline-based treatment. Also as monotherapy, if the patient has failed paclitaxel-based treatment, and if anthracycline-based treatment has either failed or cannot be continued for other reasons.
Recently, Finnish Breast Cancer Group and published in
The Lancet Oncology shows women at intermediate to high-risk of early breast cancer recurrence who received capecitabine as part of their chemotherapy regimen had a 34% reduction in the risk of the disease returning or death, compared with those taking the chemotherapy combination regimen without capecitabin. The pre-planned three-year interim analysis of a randomised, prospective trial compared adjuvant capecitabine in combination with docetaxel and cyclophosphamide plus epirubicin for the treatment of early breast cancer with the standard, non-capecitabine regimen (docetaxel, epirubicin, cyclophosphamide and fluorouracil). The analysis also found that patients taking the capecitabine-containing regimen were significantly less likely to have their cancer spread (distant metastasis) to another part of the body (a 36% reduction in risk was observed). This is the first phase III randomised trial to report efficacy of capecitabine combination therapy in the adjuvant treatment of early breast cancer.
Though capecitabine, has already been shown to be effective in patients with advanced breast cancer, but the most important conclusion the researchers have arrived is "
capecitabine-containing regimen in the early stages of breast cancer may offer survival benefits for women".....
Source :http://www.thelancet.com/journals/lanonc/article/PIIS1470-2045%2809%2970307-9/fulltext





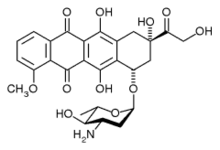 epirubicin
epirubicin

