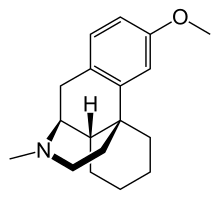
Santen Inc., the U.S. subsidiary of Santen Pharmaceutical Co., Ltd. (Santen), and UBE Corporation (UBE) announced the U.S. Food and Drug Administration (FDA) approval of Omlonti (omidenepag isopropyl ophthalmic solution) 0.002% eye drops for the reduction of elevated intraocular pressure (IOP) in patients with primary open-angle glaucoma or ocular hypertension. The approval date was September 22.
“Glaucoma prevalence is increasing as the global population ages. Supporting patients by protecting vision across the continuum of clinical care in glaucoma is a significant aim for Santen to reduce the social and economic opportunity loss of people around the world caused by eye conditions,” explains Peter Sallstig, Chief Medical Officer of Santen. “This approval is an important milestone in our ambition to tackle unmet needs in eye health and advances our goal of realization of “Happiness with Vision”. It also represents our first glaucoma offering in the U.S. We are pleased to provide doctors and patients in the U.S. with a new option to help control IOP for the more than three million Americans affected by glaucoma1 or ocular hypertension.”
“UBE Corporation is committed to working on new drug discoveries on a daily basis with the aim of providing patients with more treatment options for diseases with high unmet needs," said Yoichi Funayama, Senior Executive Officer and General Manager of the Pharmaceutical Division, UBE Corporation. “We are very pleased that this ophthalmic solution has been approved for glaucoma in the U.S., following approvals in Japan and Asia. We have high expectations that omidenepag isopropyl will provide a new treatment option for more patients suffering from glaucoma and ocular hypertension through Santen.”
Omlonti was evaluated in three randomized and controlled clinical trials in subjects with open-angle glaucoma or ocular hypertension with average baseline IOP of 24-26 mm Hg. The double-masked treatment duration was three months in all three studies. The third study included a 9-month open-label treatment period following the 3-month double-masked treatment period. In the three studies, IOP reductions were observed for all treatment arms. In the Omlonti arm, the reduction in IOP ranged from 5-7 mm Hg across all three studies. The corresponding reductions for the timolol and latanoprost arms were 5-7 mm Hg and 6-8 mm Hg, respectively.
Glaucoma causes damage to the optic nerve resulting in visual field loss, and remains a leading cause of irreversible blindness worldwide.2 Since the disease is generally progressive, early detection and treatment to control the progression are crucial, and lowering IOP is the most effective means of avoiding damage to the optic nerve. The estimated number of patients globally in 2020 was 76 million, and it is expected to increase to 95 million by 2030.3 Primary open-angle glaucoma is the most common type of glaucoma. Ocular hypertension, which affects millions, can lead to glaucoma and vision loss if untreated.4
“Treatments that focus on IOP reduction help to slow or prevent further loss of vision for those with glaucoma or ocular hypertension. However, not all patients respond to the same treatments, and some may not have successful outcomes,” said Jason Bacharach, MD, Medical and Research Director at North Bay Eye Associates, Inc. “The approval of omidenepag isopropyl ophthalmic solution 0.002% provides doctors with another safe and effective option to use when treating patients with these sight-threatening conditions.”