In continuation of my update on nilotinib

Novartis announced today that the US Food and Drug Administration (FDA) approved the inclusion of Treatment-free Remission (TFR) data in the Tasigna® (nilotinib) US product label. Tasigna is now the first and only BCR-ABL tyrosine kinase inhibitor (TKI) to include data about attempting treatment discontinuation in eligible adult patients with Philadelphia chromosome-positive chronic myeloid leukemia in the chronic phase (Ph+ CML-CP) after achieving sustained deep molecular response of MR4.5 (BCR-ABL1 International Scale [IS] <= 0.0032%) in its FDA-approved prescribing information. TFR is the ability to maintain a sustained molecular response* after stopping TKI therapy in patients with Ph+ CML-CP. TFR requires scheduled monitoring of BCR-ABL1 levels to identify possible loss of molecular response.
"It has long been our ambition at Novartis to make it possible for some people with CML to discontinue therapy," said Bruno Strigini, CEO, Novartis Oncology. "We are proud that Tasigna is now the first and only TKI with TFR data in its labeling in the US and several countries around the globe. This achievement would not have been possible without the partnership of patients around the world who participated in our groundbreaking TFR trials, helping Novartis to once again reimagine what is possible for people living with CML."
With this label update, Tasigna is the only TKI that provides defined, approved criteria to attempt and monitor TFR. This approval follows a priority review for a supplemental New Drug Application (sNDA) for Tasigna seeking the addition of TFR information and is based on safety and efficacy results from the 96-week analyses of two open label trials, ENESTfreedom and ENESTop. These trials evaluated the potential to maintain MMR (BCR-ABL1 <= 0.1%) after stopping Tasigna therapy among eligible adult patients with Ph+ CML-CP. Patients in the trials had achieved a sustained MR4.5 with Tasigna in both the first-line setting or after switching from Glivec® (imatinib). The trials demonstrated that almost half of the Ph+ CML-CP patients who discontinued Tasigna remained in TFR approximately two years after stopping treatment[1]. Among patients who did lose molecular response during the TFR phase of the trials, nearly all regained MMR when Tasigna therapy was promptly reinitiated[1]. The safety data are consistent with previously published studies and the known safety profile of Tasigna.
The TFR data in the Tasigna label approved by the FDA included the use of the MolecularMD MRDxTM BCR-ABL test, a FDA-authorized companion diagnostic validated to measure BCR-ABL transcript levels down to MR4.5. Discontinuation of Tasigna should only be attempted under the close supervision of a physician. Frequently scheduled patient monitoring after Tasigna discontinuation is required so that possible loss of MMR and MR4.0 (BCR-ABL1 IS <= 0.01%) is quickly identified and treatment re-initiation is started promptly.
Ref : https://www.novartis.com/news/media-releases/novartis-drug-tasignar-approved-fda-first-and-only-cml-therapy-treatment-free-remission-data-its-label


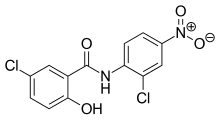





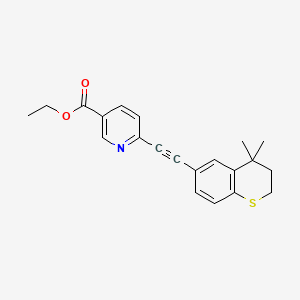 tazarotene
tazarotene