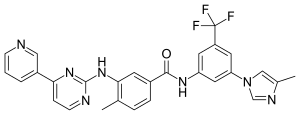
In continuation of my update on Nilotinib
Novartis announced today that the US Food and Drug Administration (FDA) expanded the indication for Tasigna (nilotinib) to include treatment of first- and second-line pediatric patients one year of age or older with Philadelphia chromosome-positive chronic myeloid leukemia in the chronic phase (Ph+ CML-CP)
In the United States, Tasigna is now indicated for the treatment of adult and pediatric patients one year of age or older with newly diagnosed Ph+ CML-CP. Tasigna is also indicated for the treatment of pediatric patients one year of age or older with Ph+ CML-CP resistant or intolerant to prior tyrosine kinase inhibitor (TKI) therapy, as well as adult patients with Ph+ CML in chronic phase and accelerated phase, resistant or intolerant to prior therapy that included imatinib.
This approval is the latest in a series of regulatory milestones that broadens the understanding and clinical use of Tasigna.
CML is a type of blood cancer where the body produces malignant white blood cells. Almost all patients with CML have an abnormality known as the "Philadelphia chromosome," which produces a protein called BCR-ABL. This protein aids the proliferation of malignant white blood cells in affected patients. Worldwide, CML accounts for approximately 3% of newly diagnosed childhood leukemia[1].
"Novartis' commitment to people living with CML is reinforced by today's FDA approval of Tasigna in children," said Liz Barrett, CEO, Novartis Oncology. "This expanded use, along with the other recent global regulatory Tasigna milestones, underscores our dedication to reimagining medicine and addressing the needs for people with CML, including children with this cancer."
The new indications, granted under the FDA's Priority Review designation, are based on two studies evaluating the efficacy and safety of nilotinib in pediatric patients (two years to less than 18 years of age) with Ph+ CML-CP. A total of 69 Ph+ CML-CP pediatric patients, either newly diagnosed (first-line) or who were resistant or intolerant to prior TKI therapy (second-line), received nilotinib[2]. In newly diagnosed pediatric patients, the major molecular response (MMR; BCR ABL/ABL <=0.1% International Scale [IS]) rate was 60.0% (95% confidence interval [CI]: 38.7, 78.9) at 12 cycles, with 15 patients achieving MMR[2]. The cumulative MMR rate among newly diagnosed pediatric patients was 64.0% by cycle 12, and the median time to first MMR was 5.6 months (range: 2.7 to 16.6). In pediatric patients with resistance or intolerance to prior TKI therapy, the MMR rate was 40.9% (95% CI: 26.3, 56.8) at 12 cycles, with 18 patients being in MMR[2]. The cumulative MMR rate among pediatric patients with resistance or intolerance was 47.7% by cycle 12, and the median time to first MMR was 2.8 months (range: 0.0 to 11.3)[2].
Adverse reactions observed in these pediatric studies were generally consistent with those observed in adults, except for laboratory abnormalities of hyperbilirubinemia (Grade 3/4: 13%)-a condition where there is too much bilirubin in the blood-and transaminase elevation (AST Grade 3/4: 1%, ALT Grade 3/4: 9%), which were reported at a higher frequency than in adult patients. One resistant or intolerant pediatric CML patient progressed to advance phase/blast crisis (AP/BC) after about 10 months on treatment.

