In continuation of my update on chloroquine

A new collaborative study led by researchers at Sanford Burnham Prebys Medical Discovery Institute (SBP) and UC San Diego School of Medicine has found that a medication used to prevent and treat malaria may also be effective for Zika virus. The drug, called chloroquine, has a long history of safe use during pregnancy, and is relatively inexpensive. The research was published today in Scientific Reports.
Zika virus remains a major global health risk. In most adults, Zika causes mild flu-like symptoms. But in pregnant women, the virus can cause serious birth defects in babies--including microcephaly--a neurological condition in which newborns have unusually small heads and fail to develop properly. There is no treatment or way to reverse the condition.
"There is still an urgent need to bolster our preparedness and capacity to respond to the next Zika outbreak," says Alexey Terskikh, Ph.D., associate professor at SBP. "Our latest research suggests the anti-malaria drug chloroquine may be an effective drug to treat and prevent Zika infections."
Terskikh is co-senior author of a new study that examined the effect of chloroquine in human brain organoids and pregnant mice infected with the virus, and found the drug markedly reduced the amount of Zika virus in maternal blood and neural progenitor cells in the fetal brain. Pregnant mice received chloroquine through drinking water in dosages equivalent to acceptable levels used in humans.
"Our research is the first to study Zika infection in a mouse model that transmits the virus in a way similar to humans," explains Alysson R. Muotri, Ph.D., professor and director of the Stem Cell Program at UC San Diego and co-senior author of the study. "Until now, researchers used a mouse strain that is deficient in interferon--a signaling protein that heightens anti-viral defenses. Those mice actually die from Zika infection, making it difficult to study the natural transmission of the virus from father and mother to fetus and to assess the effect of this transmission on the newborns.
"We believe our mouse model more accurately represents the way Zika virus infects men, women, and babies while in the womb," adds Terskikh. "Although chloroquine didn't completely clear Zika from infected mice it did reduce the viral load, suggesting it could limit the neurological damage found in newborns infected by the virus."
"In the 1950's, the Brazilian health agencies added chloroquine into cooking salt and distributed it to the population in endemic areas as an effective way of spreading the inexpensive anti-malarial drug as a prophylactic on a wide scale. This strategy was known as Pinotti's Method, named after its originator Dr. Mario Pinotti. It might be worth considering this medicated salt program one more time in Brazil", suggests Muotri.
"Chloroquine has a long history of successfully treating malaria, and there are no reports of it causing birth defects," says Terskikh. "Additional studies are certainly needed to determine the precise details of how it works. But given its low cost, availability and safety history further study in a clinical trial to test its effectiveness against Zika virus in humans is merited."
Ref : http://www.newswise.com/articles/view/685239/



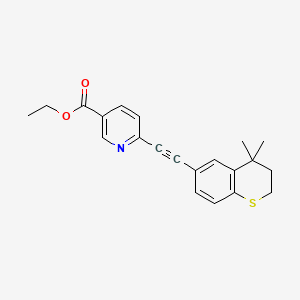 tazarotene
tazarotene