Recently, Russian researchers, led by Prof. Vladimir P. Skulachev, managed to create an antioxidant drug that selectively accumulates within mitochondria and protects them from oxidative damage. Under the trade name "Visomitin" the drug was approved for treatment of such eye diseases as cataracts and dry eye. Prof. Armen Mulkidjanian of the Faculty of Bioengineering and Bioinformatics of the Lomonosov Moscow State University and the University of Osnabrück, Germany, and his colleagues have explained why very small doses of synthetic antioxidants such as "Visomitin" could give a pronounced therapeutic effect, despite the presence of large quantities of natural mitochondrial antioxidants.
Mitochondria are intracellular structures that conduct respiration. Respiration, however, is accompanied by formation of reactive oxygen species (ROS) as by-products. The ROS are capable of damaging the mitochondria. Damaged mitochondria produce even more ROS, which can destroy cells and tissues, so that nature has special mechanisms, such as mitophagy and apoptosis, for elimination of damaged mitochondria and cells. These mechanisms are triggered after a signal of a disorder passes through the double membrane surrounding the mitochondria. Several laboratories have shown that it is possible to avoid the decay of cells and tissues by preventing the oxidation of a particular component of the mitochondrial membrane -- cardiolipin, because the oxidized molecules of cardiolipin are exactly the triggers of the signal chain.
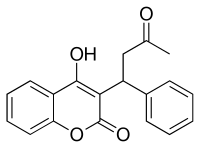
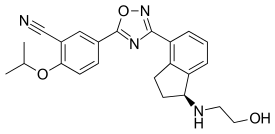
The group of Prof. Vladimir Skulachev, the Dean of the Faculty of Bioengineering and Bioinformatics and the Director of the Belozersky Institute of Physical and Chemical Biology, (the Lomonosov Moscow State University), has developed a line of mitochondria-targeted antioxidants, the so-called SkQ-ions, specifically protecting the molecules of mitochondrial cardiolipin from oxidation. In animal trials, the SkQ-ions cured inflammatory eye diseases, helped to overcome the ischemia-simulating conditions, and even reduced the manifestation of senescence. Although similarly acting drugs have been developed and studied in the US and UK laboratories, the Russian group was the first to get an approval for their drug -- as eye drops. The researchers hope that SkQ-based drugs, in the form of pills and injections, after their certification, would help to attenuate the pathological symptoms that accompany strokes, heart attacks and serious traumas.
Armen Mulkidjanian and his collaborators have managed to suggest answers to some intriguing questions. Specifically, it was not clear why cardiolipin, of all the components of the membrane, it specifically oxidized. Molecules of cardiolipin, while making only 10-20% of total membrane lipids, are specifically targeted by ROS and, after getting oxidized, trigger the self-destruction of cells. Secondly, it was not clear why the natural antioxidants, namely coenzyme Q (ubiquinol) and vitamin E (alpha-tocopherol), which are present in mitochondrial membranes in large quantities, fail in the case of cardiolipin. It remained a mystery why these substances could not protect cardiolipin from oxidation, whereas artificial, mitochondria-targeted antioxidants, designed either by the Skulachev's group in Moscow, or by their counterparts in the US and the UK, perfectly coped with this task, in spite of very small doses of the administered drugs.
Armen Mulkidjanian says that the goal of the study was set by Prof. Skulachev.
'Prof. Skulachev asked our group in Germany to tackle these puzzles,' says Armen Mulkidjanian. 'Most of the work was carried out by the post-graduate students and the employees of the Moscow University, who worked in Russia and in Germany, so that their contribution was decisive. As to the research, we have developed an experimental system to investigate quantitatively the oxidation of the cardiolipin membranes and the ability of various antioxidants to prevent it. It turned out that the SkQ-ions and the molecules of coenzyme Q protected the cardiolipin membranes from oxidation equally well, whereas vitamin E performed much worse'.
To understand why cardiolipin molecules are the main target of the ROS, the researchers compared the experimental data with their previous results and the structures of respiratory enzymes. A fraction of cardiolipin molecules is occluded within respiratory protein complexes, just those that generate ROS. 'These molecules should be the first to be oxidized,' Mulkidjanian says.
The bulky, water-insoluble molecule of coenzyme Q cannot get to these "hidden" cardiolipin molecules, as opposed to small, agile molecules of artificial antioxidants, which, as shown in the study, are capable of protecting cardiolipin molecules from oxidation by accessing them both from the membrane and from the aqueous phase.
"The essence of our work is that we have proposed a mechanism that explains how very low doses of mitochondria-targeted antioxidants could provide a distinct therapeutic effect, even being applied over large amounts of natural antioxidants, which were ineffective in this case. The mechanism should be valid for the whole class of similar drugs. We hope that our findings would help to develop new drugs,' says Armen Mulkidjanian.
Revolutionary drug explained by scientists: Scientists figured out how the world's first drug that protects the cell mitochondria from damage by aggressive oxygen can work: An international team now clarifies the molecular mechanism of a drug created in Russia and designed to prevent the damaging of cell mitochondria by reactive oxygen species.