A drug that would be the first to target the cause of Huntington's disease (HD) is effective and safe when tested in mice and monkeys, according to data released today that will be presented at the American Academy of Neurology's 68th Annual Meeting in Vancouver, Canada, April 15 to 21, 2016. A study to test the drug in humans has begun.
Huntington's disease is a rare, hereditary disease that causes uncontrolled movements, loss of intellectual abilities, emotional problems and eventually death. The disease is passed from parent to child through a mutation in the huntingtin gene. The mutation results in the production of a disease-causing huntingtin protein. Each child has a 50/50 chance of inheriting the gene mutation. Everyone who inherits the mutated gene will eventually develop the disease.
The new drug, called IONIS-HTTRx, is an antisense drug that acts as a "gene silencer" to inhibit the production of huntingtin protein in people with Huntington's disease.
"It is very exciting to have the possibility of a treatment that could alter the course of this devastating disease," said clinical study principal investigator Blair R. Leavitt, MD, of the University of British Columbia in Vancouver. "Right now we only have treatments that work on the symptoms of the disease." Leavitt notes the drug is still years away from being used in human clinical practice.
Earlier studies in mouse models of Huntington's disease showed that treatment with antisense drugs delays disease progression and results in sustained reversal of the disease phenotype. In YAC128 mice, a transgenic model of HD, motor deficits improved within one month of initiating antisense treatment and were restored to normal at two months after treatment termination. Motor skills of antisense-treated BACHD mice, another transgenic model of HD, improved eight weeks after initiation of treatment and persisted for at least nine months after treatment termination. In monkeys, dose-dependent reductions in HTT mRNA and Htt protein throughout the central nervous system were observed after intrathecal administration of an antisense drug. Reduction of cortical huntingtin levels by 50 percent was readily achieved in monkeys and correlated with 15 to 20 percent reduction in the caudate. In further tests in rodents and monkeys, IONIS-HTTRx was found to be well-tolerated without any dose-limiting side effects.

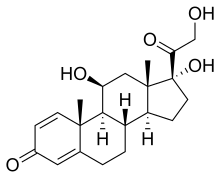 (Prednisole)
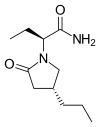
(Prednisole) (Indomethacin)
(Indomethacin)
 (
( (Donepezil)
(Donepezil) 

 (Elbasvir)
(Elbasvir)  (Grazoprevir)
(Grazoprevir)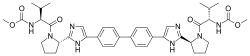
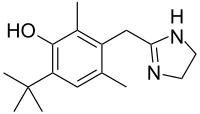
 Tetracaine
Tetracaine