Monday, September 13, 2010
Synthetic derivative of Retinoic acid can induce cell death
Saturday, January 25, 2020
FDA Approves Inrebic (fedratinib) for the Treatment of Patients With Myelofibrosis

“The approval of Inrebic is another important milestone for Celgene and underscores our commitment to people living with blood cancers,” said Jay Backstrom, M.D., M.P.H., Chief Medical Officer for Celgene. “We are excited to provide Inrebic as a new treatment option that may be used in patients with myelofibrosis, including patients previously treated with ruxolitinib.”
“Myelofibrosis can cause patients to suffer in many ways, including experiencing debilitating symptoms,” said Ruben Mesa, M.D., FACP, Director of the Mays Cancer Center at UT Health San Antonio Cancer Center MD Anderson. “There has not been a new treatment approved for this disease in nearly a decade. With Inrebic, physicians and patients now have another option available for myelofibrosis.”
“Inrebic is a much-welcomed new treatment for the myelofibrosis community,” said Ann Brazeau, Chief Executive Officer and Founder, MPN Advocacy and Education International. “This FDA approval marks an important milestone for people living with myelofibrosis as we embark on making greater strides in the diagnosis, understanding and treatment of this disease.”
Wednesday, December 28, 2016
Metabolite of oral DMF drug for multiple sclerosis appears to slow onset of Parkinson's disease
 dimethylfumarate
dimethylfumarate Saturday, September 10, 2011
Researchers rethink fenretinide for prevention of oral cancer
Friday, December 23, 2016
One-third of osteoporotic women taking oral bisphosphonates have elevated risk for bone fracture

"We know that taking bisphosphonates decrease fracture risk compared to those not taking these drugs," Dr. Imel said. "But what about those women who weren't getting the anticipated benefit and are not improving bone density or even are losing bone density? What predicted that? The purpose of this study was to focus attention on those not doing well, in order to begin to decrease the odds of future fractures in this large group of vulnerable patients.
"Not everyone responds the same way to oral bisphosphonates or any drug. Various factors could convey continued risk of fracture in spite of bisphosphonate therapy, including other medical problems and risk factors for falling. Since we know that such a high percentage of women continue to have elevated fracture risk we -- doctors and patients -- need to focus on these factors," Dr. Imel said. "For example, we found that women who had other medical conditions in addition to low bone density--a frequent occurrence in this older population--had higher fracture risk. Taking some medications in combination with bisphosphonates seemed to increase fracture risk. However, having more medical conditions and taking more drugs are most likely markers of heightened risk rather than causative factors."
"I always tell my osteoporosis patients, 'Don't fall,'" said Dr. Imel. "They usually chuckle, and then we talk about things they can do to decrease the risk of falling, including proper footwear and assistive devices. Many patients are reluctant to use a cane or a walker. I try to get them to understand the importance of using any tool that decreases the chance of falling."
Friday, April 13, 2018
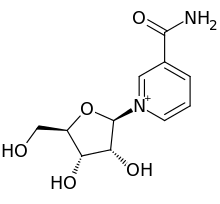
Compound prevents neurological damage, shows cognitive benefits in mouse model of Alzheimer’s disease
“The pursuit of interventions to prevent or delay Alzheimer’s and related dementias is an important national priority,” said Richard J. Hodes, M.D., director of the NIA. “We are encouraging the testing of a variety of new approaches, and this study’s positive results suggest one avenue to pursue further.”
“We are encouraged by these findings that see an effect in this Alzheimer’s disease model,” said Dr. Bohr. “We are looking forward to further testing of how NR or similar compounds might be pursued for their possible therapeutic benefit for people with dementia.”
Friday, November 13, 2015
Research finding offers hope for more powerful aspirin-like drugs
Monday, December 12, 2016
Walnuts may improve your colon health: Eating walnuts changes the gut microbiome and reduces cancer growth, study shows
Sunday, July 17, 2011
Tocotrienol could help reduce stroke damage
Tuesday, October 4, 2022
Daily Multivitamin May Protect Against Cognitive Decline in Older Adults
A daily multivitamin may provide cognitive benefits for older adults, according to a study published online Sept. 14 in Alzheimer’s & Dementia.
Laura D. Baker, Ph.D., from the Wake Forest University School of Medicine in Winston-Salem, North Carolina, and colleagues assessed whether daily use of cocoa extract (containing 500 mg/day flavanols) versus placebo and a commercial multivitamin-mineral (MVM) versus placebo improved cognition in 2,262 older women and men (mean age, 73 years).
The researchers found that cocoa extract had no effect on global cognition. However, compared with placebo, daily MVM supplementation resulted in a statistically significant benefit on global cognition, with a more pronounced effect seen in participants with a history of cardiovascular disease. Benefits of MVM were also seen for memory and executive function. There were no significant interactions observed between cocoa extract and MVM for any of the cognitive composites.
"Our study showed that although cocoa extract did not affect cognition, daily multivitamin-mineral supplementation resulted in statistically significant cognitive improvement. This is the first evidence of cognitive benefit in a large longer-term study of multivitamin supplementation in older adults," Baker said in a statement. "It's too early to recommend daily multivitamin supplementation to prevent cognitive decline. While these preliminary findings are promising, additional research is needed in a larger and more diverse group of people."
Saturday, April 7, 2012
Immunotherapy and Chemotherapy Regimen May Prolong Survival in Advanced Cancers
Friday, December 6, 2013
Health Benefits of Ragi | Medindia
Thursday, August 10, 2017
Walnuts could be key to happier state-of-mind in young healthy men
Ref: http://news.unm.edu/news/the-key-to-a-better-mood-for-young-men-is-a-nut
Read more at ..





