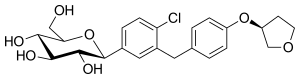
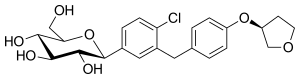
 empagliflozin
empagliflozin  Metformin
Metformin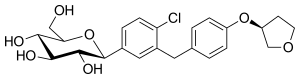 empagliflozin
empagliflozin  Metformin
Metformin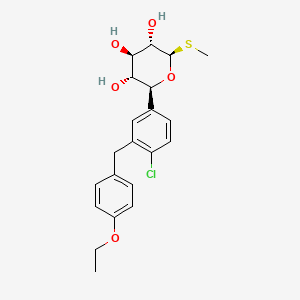
“We believe in the overall benefit-risk profile of sotagliflozin for adults with type 1 diabetes who lack adequate glycemic control using insulin alone,” said Rachele Berria, MD, PhD, Global Vice President and Head of Diabetes Medical Affairs, Sanofi. “We will continue to work with the FDA through its review process to hopefully bring to patients a new treatment that can help people living with type 1 diabetes control their blood sugar and address some of the challenges of insulin-only therapy.”
“In clinical trials, when used in combination with insulin therapy, sotagliflozin significantly improved glycemic control without increasing hypoglycemia,” said Pablo Lapuerta, MD, Executive Vice President and Chief Medical Officer, Lexicon. “These results could not be achieved with insulin alone. Diabetic ketoacidosis is an inherent risk of type 1 diabetes and an increase was seen with sotagliflozin compared to insulin alone. We believe this can potentially be addressed with proper education and monitoring.”
Specifically, in two new studies recently published in the Journal of Clinical Medicine and Pharmaceuticals, researchers have developed an obese and diabetic rodent model and have shown that melatonin protects from kidney damage caused by diabesity.
The scientists have shown that chronic administration of melatonin at doses (10 mg/kg body weight/day) prevents mitochondrial and endoplasmic reticulum disruption, which play a critical role in the development and pathogenesis of kidney cell (nephron) damage, and its progression to renal failure.
Thus, it has been shown that melatonin prevents the impairment of the function and dynamics of cellular mitochondria, decreasing the increased production of oxygen free radicals (responsible for oxidative stress). It also prevents pathological alteration in the function of the endoplasmic reticulum (another cell cytoplasmic organelle), which, in conditions of abnormally high oxidative stress, is related to an increase in programmed cell death (of the nephron) leading to the loss of renal functionality, as a preliminary step to the development of renal failure and the need for hemodialysis or transplantation.
The studies coordinated by the UGR show the efficacy of melatonin in halting the progression of renal damage mediated by mitochondrial damage and excess endoplasmic reticulum stress.
As the lead author of this study, Ahmad Agil, a researcher at the Department of Pharmacology of the UGR, says, "Kidney damage is caused by metabolic complications of obesity, such as diabetes, hypertension, blood lipid disorders or fatty liver disease. Given that the prevalence of these pathologies (collectively recognized as metabolic syndrome) continues to increase, kidney damage and its progression over time to kidney failure has become a health problem that affects millions of people worldwide, with a great socioeconomic cost, requiring hemodialysis facilities and/or kidney transplant services, with the corresponding compatibility studies required."
The importance of the work lies not only in the efficacy of melatonin in counteracting the two proposed mechanisms of renal damage (based on the alteration of mitochondrial function and dynamics and the function of the endoplasmic reticulum (ER)), but they also propose an alternative preventive treatment that would improve this renal function with a well-studied drug with a very high safety profile such as melatonin, which is a drug that in the EU must be prescribed by a doctor and is already administered in the treatment of insomnia.
The new findings have also been associated with an improvement in glomerular filtration rate and renal damage of the nephron, manifested in a decrease in creatinine clearance levels (the best marker of renal function), proteinuria, and in the improvement of renal structure, observed after histopathological study of the kidney.
These results are in line with those previously published by these researchers in the last 10 years, demonstrating that the pharmacological administration of melatonin constitutes another new strategy in the therapeutic approach to diabesity (central obesity and its type 2 diabetes) and its complications (such as hepatic steatosis, hypertension, lipid alteration, etc.).
"Our main challenge is the application of melatonin and other strategies such as intermittent fasting in the field of medicine, especially to address the possibility of a treatment perspective for the aforementioned pathologies (diabesity and its complications) that involve an increase in oxidative stress, and mitochondrial damage and associated meta-inflammation (inflammation of metabolic origin)," Agil says.
According to the results, melatonin could help treat kidney damage, which establishes the need to develop new clinical trials to test its effectiveness in humans. The next step is to investigate how it helps in the maintenance of mitochondrial and endoplasmic reticulum homeostasis, and to a greater extent, if melatonin therapy would allow delaying or stopping progressive renal damage by promoting its chronic pharmacological use in kidney repair and regeneration.
 metformin
metformin 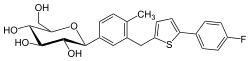 canagliflozin
canagliflozin“The FDA encourages drugs to be made available to the widest number of patients possible when there is evidence of safety and efficacy,” said Lisa Yanoff, M.D, acting director of the Division of Metabolism and Endocrinology Products in the FDA’s Center for Drug Evaluation and Research. “Victoza has now been shown to improve blood sugar control in pediatric patients with type 2 diabetes. The expanded indication provides an additional treatment option at a time when an increasing number of children are being diagnosed with this disease.”


"Semaglutide is a potent once-weekly glucagon-like peptide 1 receptor agonist, reducing significantly HbA1c, body weight, and systolic blood pressure. However, it is associated with increased incidence of gastrointestinal adverse events," the authors write.
"Cardiovascular disease is a leading cause of death in adults with type 2 diabetes mellitus," said Jean-Marc Guettier, M.D., C.M., director of the Division of Metabolism and Endocrinology Products in FDA's Center for Drug Evaluation and Research. "Availability of antidiabetes therapies that can help people live longer by reducing the risk of cardiovascular death is an important advance for adults with type 2 diabetes."
We are very excited about this new drug combination because for the first time ever, we are able to see rates of human beta cell replication that are sufficient to replenish beta cell mass in humans with diabetes."Andrew Stewart, MD, Director of the Mount Sinai Diabetes, Obesity, and Metabolism Institute and lead author of the study

Finding progesterone on the list was a promising validating step. Four of the drugs on our list have seen effectiveness in past studies that were either experimental or retrospective. This leads us to believe in the biology behind the identification of these drugs."Brian Le, PhD, postdoctoral scholar in the UCSF Department of Pediatrics and the Bakar Computational Health Sciences Institute, and the first author of the study