A compound found in citrus oils could help alleviate dry mouth caused by radiation therapy in head and neck cancer patients, according to a new study by researchers at the Stanford University School of Medicine.
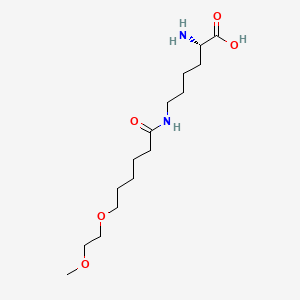
The compound, called d-limonene, protected cells that produce saliva in mice exposed to radiation therapy—without diminishing the tumor-fighting effects of the radiation. The researchers, led by graduate student Julie Saiki, also showed that d-limonene taken orally is transported to the salivary gland in humans.
The study will be published online May 21 in the Proceedings of the National Academy of Sciences.
The finding was possible because of a close collaboration between clinicians and basic scientists, said co-senior author Daria Mochly-Rosen, Ph.D., professor of chemical and systems biology. "This is a perfect example of two pieces that could not work alone."
"Stanford is a fertile ground for collaboration," added Quynh-Thu Le, co-senior author and professor and chair of radiation oncology.
About 40 percent of head and neck cancer patients who receive radiation therapy develop dry mouth, known clinically as xerostomia. It's more than uncomfortable: patients struggle to speak and swallow and are more likely to develop oral pain or dental cavities, and the condition can lead to tooth removal in some cases, Le said. And, although some recovery can occur in the first years after the therapy, once saliva production is impaired, it is usually gone for life.
Radiation can kill salivary cells
One drug, called amifostine, is approved for use during radiation therapy to try to ward off dry mouth, but its side effects, including nausea and potential low blood pressure, are common, so it is rarely used in the clinic, Le said.
Many of the saliva-producing cells that are needed to keep the mouth constantly moist are found in a pair of structures called the submandibular glands, tucked under the lower jawbone on each side of the chin. Radiation often kills these cells and, more troublingly, also salivary stem and progenitor cells, those juvenile members of the population that are needed to rebuild and restore the capacity to make saliva.
The key to retaining salivary function is protecting these rare but critical stem and progenitor cells. That's tricky because, following radiation therapy, toxic, highly reactive compounds called aldehydes are created in the gland, gumming up cellular function.
Le, the Katharine Dexter McCormick and Stanley McCormick Memorial Professor, who specializes in treating head and neck cancer, said she had spent a decade hearing from her patients about their struggles with dry mouth. "I wanted to do something," she said.
Her initial strategy was to try to regenerate salivary stem cells and, while working with these cells, her lab found that they contain high levels of an enzyme called aldehyde dehydrogenase 3A1, or ALDH3A1. The enzyme is a member of the large aldehyde dehydrogenase family of enzymes, proteins that initiate or speed up chemical reactions, that can defang troublesome aldehydes. But ALDH3A1 isn't a match for the radiation-unleashed aldehydes on its own.
She needed to find something to amp it up.
Looking to the East
Le had met with Mochly-Rosen through SPARK, a program founded and co-directed by Mochly-Rosen, that shepherds basic science discoveries into the clinic. Mochly-Rosen, who is the George D. Smith Professor in Translational Medicine, had been working on aldehyde dehydrogenases for more than a decade and had obtained access to a library of 135 traditional Chinese medicine extracts.
Many of those extracts have been used as treatments for various ailments in humans for hundreds of years, boosting the likelihood they are safe to use, Mochly-Rosen said.
Her team found that seven of these 135 extracts boosted ALDH3A1 activity. It was up to Saiki to see if she could break apart these complex natural extracts—from plants including tangerine, lotus and an Asian rhizome known as zhi mu in Chinese—to find out what, exactly, was activating the enzyme.
"She did the unthinkable, a really amazing achievement. She found the single active ingredient that activates the enzyme, ALDH3A1," Mochly-Rosen said.
Admittedly, Mochly-Rosen and Saiki said, a bit of luck and a fair amount of trial-and-error were involved. D-limonene stood out from other compounds in the extracts because it is broken down relatively quickly in the body and has been deemed by the Food and Drug Administration as a food flavor "generally recognized as safe" that has been approved for use as a food additive, Saiki said.
Saiki said she was pleasantly surprised by her finding. "It's a very common molecule, and sometimes as a scientist you wonder, Why hasn't anyone seen this before?" she said.
Next, they had to see if d-limonene would rev up ALDH3A1 in living cells.
Testing in mice, and humans
A series of experiments with mouse cells that had been exposed to radiation showed that d-limonene reduced aldehyde concentrations in both adult and salivary stem and progenitor cells. Even when the cells were treated weeks after radiation exposure, d-limonene still improved their ability to recover, repair gland structure and produce saliva. Mice that ate d-limonene and were exposed to radiation also produced more saliva than mice that did not receive d-limonene and were exposed to radiation. The researchers also learned that d-limonene wasn't likely to boost saliva production so high that mice, or humans, would be drooling—the compound didn't increase saliva production in mice that hadn't been exposed to radiation. And they confirmed that d-limonene did not affect tumor growth or interfere with the tumor-shrinking effects of the radiation in mice.
A further set of experiments pulled back the curtain on d-limonene's work: it was stopping the expression of messages that trigger the salivary stem and progenitor cells to self-destruct.
Buoyed by these positive results, the researchers wanted to know if the compound had any hope of helping patients. To work, it would have to be active inside the salivary glands. To find out, they launched a phase-0 study, an early clinical trial in a small number of patients to see if d-limonene, taken by mouth in a capsule, would be distributed to the salivary gland. Four participants who were having a salivary gland tumor removed took d-limonene for two weeks before the surgery. When the tissue was examined after it was removed, researchers found high levels of d-limonene, showing that it has the potential to be used therapeutically in humans—it reaches the salivary gland tissue.
The patients did experience one quirky side effect: Citrus-infused burps.
Next, the team plans to start the clinical trial process, which will take several years and require a multi-institutional collaboration, Le said. "If it works, then this type of drug would be used safely to prevent dry mouth in patients in the long run and make it much easier for patients to tolerate the radiation treatment with an improved quality of life after the treatment," she said.
The work is an example of Stanford Medicine's focus on precision health, the goal of which is to anticipate and prevent disease in the healthy and precisely diagnose and treat disease in the ill.
Ref : http://med.stanford.edu/news/all-news/2018/05/citrus-oil-compound-could-reduce-dry-mouth-in-cancer-treatment.html