In continuation of my update on imiquimod and fluorouracil
Basal cell carcinoma is one of the most common cancers and its incidence is increasing worldwide, putting a significant burden on health services. Topical treatments are available for superficial basal cell carcinoma (BCC) but there has a lack of long-term follow-up data to guide treatment decisions. A three-year randomized controlled clinical trial has found that two topical creams are effective in most primary, low-risk superficial BCC, comparing favorably with photodynamic therapy (PDT), as reported by investigators in the Journal of Investigative Dermatology.
More than 80% of all skin cancers are BCC, arising from the basal cells (i.e., small, round cells found in the lower layer of the epidermis). There are over two million cases a year in the U.S. and the lifetime risk of developing a BCC before the age of 85 years is one in five people. The prognosis is excellent, but it can cause significant disfigurement by invading surrounding tissues.
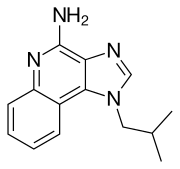
While most types of BCC require surgery, superficial BCC can be treated topically with noninvasive treatments such as PDT, imiquimod cream, fluorouracil cream, cryosurgery or electrodessication and curettage.
Investigators in the Netherlands report the results of a three-year follow-up of a randomized controlled trial that compared three noninvasive treatments that included imiquimod and fluorouracil cream. "The main advantages of noninvasive treatments are good cosmetic outcome, preservation of surrounding tissue, and potential for home application of either creams," explained lead investigator Marieke Roozeboom of the Department of Dermatology, Maastricht University Medical Center in the Netherlands. "Throughout the last two decades there has been a growing interest in these non-surgical therapies, which offer the possibility of avoiding surgery and reducing demands on busy medical practices."
However, prior to this study there has been a lack of randomized controlled trials with a long-term follow-up that compare the effectiveness of noninvasive treatments. Consequently, there is no consensus in international BCC guidelines on the first choice of noninvasive therapy for superficial BCC.
A total of 601 patients with a superficial BCC participated in this study: 202 patients were treated with methylaminolevulinate photodynamic therapy (MAL-PDT), 198 with imiquimod cream, and 201 with fluorouracil cream. The three study groups had a similar distribution of baseline characteristics, with the exception of tumor size.
Around 80% of patients with superficial BCC were tumor free after imiquimod treatment after three years. The clearance rate was 68% for patients treated with fluorouracil and 58% for individuals receiving PDT.
 imiquimod
imiquimod  fluorouracil
fluorouracil"Based on our findings, both imiquimod and fluorouracil are effective noninvasive treatments in most primary, low-risk superficial BCC, but the data provide no definite evidence for superiority of imiquimod to fluorouracil," commented Dr. Roozeboom. "Both creams have an equal cosmetic outcome and risk of local adverse events. Fluorouracil has the advantage of being less expensive than imiquimod. However, between one- and three-year follow-up, more recurrences were diagnosed in the fluorouracil group compared with the imiquimod group."

