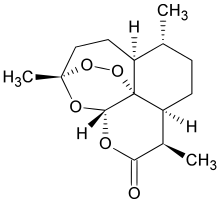
In continuation of my update on artemisinin
A team of researchers has uncovered the mystery behind the potent parasite-killing effect of artemisinin, a drug that is considered to be the last line of defense against malaria. Given the emergence of artemisinin resistance, these findings could potentially lead to the design of new treatments against drug-resistant parasites.
Assistant Professor Lin Qingsong, who is from the Department of Biological Sciences under the NUS Faculty of Science and is one of the scientists who led the study, explained, "Many people may not realise that more human lives are lost to the tiny mosquito, more specifically malaria parasites, each year as compared to ferocious animals such as lions and sharks. After infection, malaria parasites, known for their blood-eating nature, can propagate inside the human body rapidly and consume up to 80 per cent of red blood cells in a short period of time, leading to a series of deadly symptoms."
About 3.2 billion people -- almost half of the world's population -- are considered to be at risk of malaria by the World Health Organization. As of September 2015, there were an estimated 214 million cases of malaria and 438,000 malaria-linked deaths this year alone.
Artemisinin and its derivatives are currently the most potent class of anti-malarial drugs. In recognition of its importance against malaria, the discovery of artemisinin won Chinese scientist Ms Tu Youyou the 2015 Nobel Prize in Physiology or Medicine earlier in October this year. While there have been extensive studies on artemisinin, the mechanism of the drug is not well understood.
Asst Prof Lin, together with Dr Wang Jigang, who was formerly with the NUS Department of Biological Sciences and now with the Singapore-MIT Alliance for Research & Technology, Associate Professor Kevin Tan from the Department of Microbiology and Immunology at the NUS Yong Loo Lin School of Medicine and their research team, discovered over 120 protein targets of artemisinin, and the mechanism that activates its deadly killing effect. The findings of the study are published in the journal Nature Communications on 23 December 2015.




