Merck & Co., Inc. , announced that the U.S. Food and Drug Administration (FDA) has approved Prevymis (letermovir) once-daily tablets for oral use and injection for intravenous infusion. Prevymis is indicated for prophylaxis (prevention) of cytomegalovirus (CMV) infection and disease in adult CMV-seropositive recipients [R+] of an allogeneic hematopoietic stem cell transplant (HSCT).
CMV is a common and potentially serious viral infection in allogeneic HSCT recipients. CMV-seropositive patients who undergo an HSCT are at high risk for CMV reactivation. Any level of CMV infection is associated with increased mortality in HSCT patients.
In the pivotal Phase 3 clinical trial supporting approval, significantly fewer patients in the Prevymis group (38%, n=122/325) compared to the placebo group (61%, n=103/170) developed clinically significant CMV infection, discontinued treatment or had missing data through Week 24 post-HSCT [treatment difference: -23.5 (95% confidence interval -32.5 to -14.6), (p<0.0001)], the primary efficacy endpoint. All-cause mortality in patients receiving Prevymis was lower compared to placebo, 12% vs. 17%, respectively, at week 24 post-transplant. In this study, the incidence of bone marrow suppression in the Prevymis group was comparable to the placebo group. The median time to engraftment was 19 days in the Prevymis group and 18 days in the placebo group.
Prevymis is contraindicated in patients receiving pimozide or ergot alkaloids. Increased pimozide concentrations may lead to QT prolongation and torsades de pointes. Increased ergot alkaloids concentrations may lead to ergotism. Prevymis is contraindicated with pitavastatin and simvastatin when co-administered with cyclosporine. Significantly increased pitavastatin or simvastatin concentrations may lead to myopathy or rhabdomyolysis.
The concomitant use of Prevymis (letermovir) and certain drugs may result in potentially significant drug interactions, some of which may lead to adverse reactions (Prevymis or concomitant drugs) or reduced therapeutic effect of Prevymis or the concomitant drug. Consider the potential for drug interactions prior to and during Prevymis therapy; review concomitant medications during Prevymis therapy; and monitor for adverse reactions associated with Prevymis and concomitant medications.
“Our findings demonstrate that letermovir is a significant and welcomed advance in the prevention of clinically significant CMV infection and lowers mortality in this highly vulnerable patient population,” said Dr. Francisco M. Marty, associate professor of medicine at Harvard Medical School and attending physician in transplant and oncology infectious diseases at Dana-Farber Cancer Institute and Brigham and Women’s Hospital in Boston.
The recommended dosage of Prevymis is 480 mg administered once daily, initiated as early as Day 0 and up to Day 28 post-transplantation (before or after engraftment), and continued through Day 100 post-transplantation. If Prevymis is co-administered with cyclosporine, the dosage of oral or intravenous Prevymis should be decreased to 240 mg once daily. Prevymis is available as 240 mg and 480 mg tablets, which may be administered with or without food. Prevymis is also available as 240 mg and 480 mg injection for intravenous infusion via a peripheral catheter or central venous line at a constant rate over one hour.
“Prevymis is the first new medicine for CMV infection approved in the U.S. in 15 years,” said Dr. Roy Baynes, senior vice president, head of clinical development, and chief medical officer, Merck Research Laboratories. “Prevymis continues Merck’s longstanding tradition of bringing forward important new therapies to address serious infectious diseases. We are proud to add this breakthrough medicine to our existing offerings for physicians and patients.”
Prevymis is expected to be available in December. The list price (wholesaler acquisition cost) per day for Prevymis tablets is $195.00 and for Prevymis injection is $270.00. Wholesaler acquisition costs do not include discounts that may be paid on the product.
The cardiac adverse event rate (regardless of investigator-assessed causality) was higher in patients receiving Prevymis than placebo (13% vs. 6%). The most common cardiac adverse events were tachycardia (reported in 4% Prevymis patients and 2% placebo patients) and atrial fibrillation (reported in 3% Prevymis patients and 1% placebo patients). These adverse events were reported as mild or moderate in severity. The rate of adverse events occurring in at least 10% of Prevymis-treated HSCT recipients and at a frequency at least 2% greater than placebo were nausea (27% vs. 23%), diarrhea (26% vs. 24%), vomiting (19% vs. 14%), peripheral edema (14% vs. 9%), cough (14% vs. 10%), headache (14% vs. 9%), fatigue (13% vs. 11%), and abdominal pain (12% vs. 9%). The most frequently reported adverse event that led to study drug discontinuation was nausea (occurring in 2% of Prevymis patients and 1% of placebo patients). Hypersensitivity reaction, with associated moderate dyspnea, occurred in one patient following the first infusion of IV Prevymis after switching from oral PREVYMIS, leading to treatment discontinuation.
Ref : https://www.drugs.com/history/prevymis.html






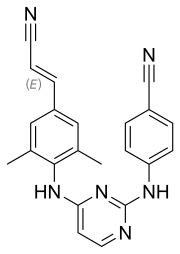 rilpivirine
rilpivirine  Dolutegravir
Dolutegravir