University of Colorado Boulder researchers have discovered a potent, drug-like compound that could someday revolutionize treatment of rheumatoid arthritis and other autoimmune diseases by inhibiting a protein instrumental in prompting the body to start attacking its own tissue.
"We have discovered a key to lock this protein in a resting state," said Hang Hubert Yin, a biochemistry professor in the BioFrontiers Institute and lead author of a paper, published today in Nature Chemical Biology, describing the discovery. "This could be paradigm shifting."
More than 23.5 million Americans suffer from autoimmune diseases like rheumatoid arthritis, scleroderma and lupus, in which an overzealous immune response leads to pain, inflammation, skin disorders and other chronic health problems.
Three of the top five selling drugs in the United States aim to ease their symptoms. But no cure exists, and treatments are expensive and come with side effects.
"Given the prevalence of these diseases, there is a big push for alternatives," Yin said.
For years, scientists have suspected that a protein called Toll-like receptor 8 (TLR8) plays a key role in the innate immune response. When it senses the presence of a virus or bacteria, it goes through a series of steps to transform from its passive to active state, triggering a cascade of inflammatory signals to fight off the foreign invader. But, as Yin explained, "it can be a double-edged sword" leading to disease when that response is excessive.
Because TLR8 has a unique molecular structure and is hidden inside the endosome -- an infinitesimal bubble inside the cell -- rather than on the cell's surface, it has proven an extremely difficult target for drug development.
"This is a long-sought-after target with very little success," Yin said.
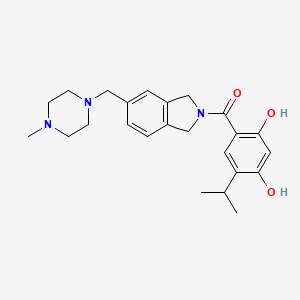
But his study shows a drug-like molecule called CU-CPT8m binds to and inhibits TLR8 and exerts "potent anti-inflammatory effects" on the tissue of patients with arthritis, osteoarthritis and Still's disease, a rare autoimmune illness.
For the study, Yin and his co-authors used high-throughput screening to look through more than 14,000 small molecule compounds to determine whether they had the right chemical structure to bind to TLR8. They identified four that shared a similar structure.
Using that structure as a model, they chemically synthesized hundreds of novel compounds in an effort to find one that perfectly bound to and inhibited TLR8.
Previous efforts to target the protein have focused on shutting it down when it is in its active state. But the compound Yin discovered prevents it from activating while still in its passive state.
"Before, people were trying to close the open door to shut it down. We found the key to lock the door from the inside so it never opens," Yin said.
Much more research is necessary, but that could lead to treatments that strike at the root cause of autoimmune diseases, rather than just treating symptoms.
With help from CU's Technology Transfer Office, Yin has already filed a patent application and hopes to move on to animal studies and clinical trials within the next two years.
In the meantime, the new compound can serve as a first-of-its kind tool to understand exactly what TLR8 and the other nine toll-like receptors do in the body.
"Our study provides the first small molecule tool to shut this protein down so we can understand its pathogenesis," Yin said.
Ref : https://www.colorado.edu/today/2017/11/20/arthritis-autoimmune-disease-discovery-could-lead-new-treatments


 rilpivirine
rilpivirine  Dolutegravir
Dolutegravir