Combination therapy with two immunotherapy drugs produces an unprecedented doubling of response rates from 20 percent to 40 percent, a new study shows.
The multicenter trial involving 100 patients showed that the addition of ipilimumab to nivolumab, which is currently FDA-approved for treatment of kidney cancer, leads to responses that can last beyond two years. Half of the patients in the study, which appears in the Journal of Clinical Oncology, had metastases that had grown while they were on previous therapy.
"For this group of patients, these are very significant results," said lead author Dr. Hans Hammers, Associate Professor of Internal Medicine and co-leader of the Kidney Cancer Program at the Harold C. Simmons Comprehensive Cancer Center of UT Southwestern Medical Center.
The results set the stage for a pivotal Phase III trial, which has completed enrollment of patients. Should the results of this study be repeated in the larger Phase III trial, it would lead to a new standard of care for kidney cancer patients, said Dr. Hammers, formerly of Johns Hopkins medical system, who holds the Eugene P. Frenkel, M.D. Scholar in Clinical Medicine at UT Southwestern.
While significant advances in the treatment for kidney cancer over the last decade have led to the approval of a dozen drugs, these drugs are mostly palliative, lacking the potential for cure. "By contrast, durable responses lasting many years can be achieved with immunotherapy," said Dr. Hammers.
Activation of the immune system, however, can lead to serious complications, requiring potent anti-inflammatory drugs. "While side effects of immunotherapy can be significant, they are typically reversible, and unlike current therapies, don't significantly dampen patients' daily quality of life," said Dr. Hammers.
"Given the potential severity of the adverse effects, patients benefit from expert management available at centers of excellence," said Dr. James Brugarolas, Associate Professor of Internal Medicine and Leader of the Kidney Cancer Program at UT Southwestern.
Ongoing efforts in the Kidney Cancer Program focus on leveraging Nobel Prize-winning discoveries from UT Southwestern's Dr. Bruce Beutler leading to a new family of proteins that activate the immune system, the toll-like receptors. "Another avenue we are exploring, is the combination of immunotherapy and radiation," said Dr. Brugarolas.
Nobel Laureate Dr. Beutler, Regental Professor and Director of the Center for the Genetics of Host Disease, discovered an important family of receptors that allow mammals to sense infections when they occur, triggering a powerful inflammatory response. For this work, he received the 2011 Nobel Prize in Physiology or Medicine. Dr. Beutler, also Professor of Immunology, holds the Raymond and Ellen Willie Distinguished Chair in Cancer Research, in Honor of Laverne and Raymond Willie, Sr.
Kidney cancer is the sixth most common cancer type affecting both men and women. Classic chemotherapy has never worked well for kidney cancer. Targeted therapies have prolonged life expectancy, but are associated with daily side effects. Single-agent immunotherapies improve patients' survival, but only benefit a subset of patients. Combination immunotherapy with nivolumab and ipilimumab as tested in the kidney cancer study described here is already FDA-approved for treatment of melanoma, and is being tested for other cancers.
The Kidney Cancer Program at UTSW is one of two programs in the U.S. recognized with a Specialized Program of Research Excellence award by the National Cancer Institute. Discoveries at the Kidney Cancer Program have led to a new understanding of how kidney cancer develops and are leading to new treatments.
The Harold C. Simmons Comprehensive Cancer Center is the only NCI-designated Comprehensive Cancer Center in North Texas and one of just 48 NCI-designated Comprehensive Cancer Centers in the nation. Simmons Comprehensive Cancer Center includes 13 major cancer care programs. In addition, the Center's education and training programs support and develop the next generation of cancer researchers and clinicians. Simmons Comprehensive Cancer Center is among only 30 U.S. cancer research centers to be designated by the NCI as a National Clinical Trials Network Lead Academic Participating Site.





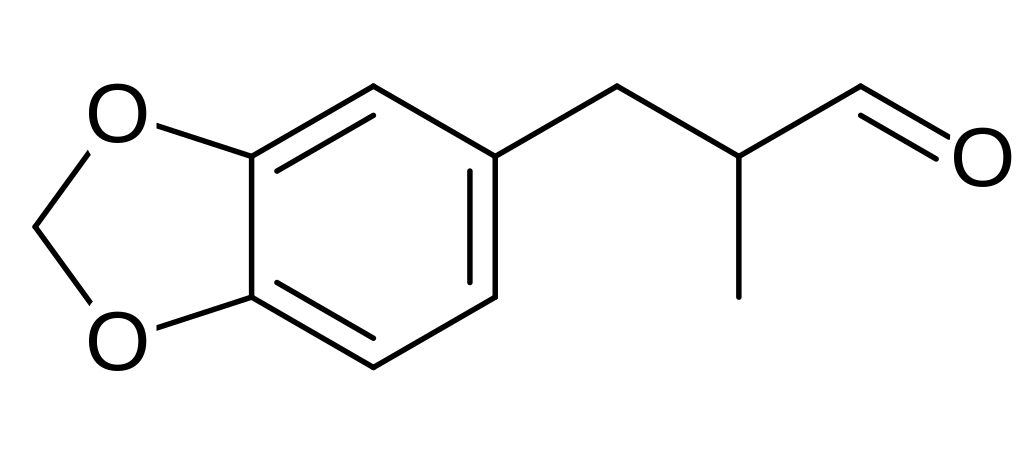
 Capsaicin
Capsaicin




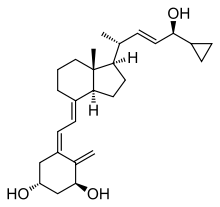 Calcipotriol
Calcipotriol