Stuttering, an interruption in the flow of speech, affects about three million Americans. It begins most often in childhood, affecting four men for every woman. A precise cause of this complex communicative disorder is not known.
A genetically influenced condition, stuttering appears to originate when various aspects of a young child's development interact, and is best addressed with early intervention. No cure for it has been found, but behavioral treatment options are available. Currently, no Food and Drug Administration (FDA)-approved drug treatments are available.

In an attempt to find a new medicine, a research team at the School of Medicine at the University of California, Riverside, in partnership with the speech pathology laboratory at the University of Redlands, will conduct a study at CITrials in Riverside, Calif., to determine how effective ecopipam, an orally administered medication, is as treatment against stuttering.
Ten volunteers will be selected to participate in the FDA-approved clinical trial. The study, scheduled to begin next month, is seeking volunteers, although space is limited. People interested in participating in the study may contact Gerald Maguire, M.D., the chair of psychiatry and neuroscience at UC Riverside and the associate dean for graduate medical education, who is leading the study: gerald.maguire@medsch.ucr.edu.
"The study is exploratory," Maguire said. "We are the only site in the world conducting this trial; ecopipam has never been tested for stuttering. It has been tested for treatment of tics in Tourette syndrome, a neurological disease, with some encouraging results. Stuttering shares some similarities to the vocal changes seen in subjects with Tourette syndrome. We are hopeful ecopipam will yield beneficial effects in stuttering."
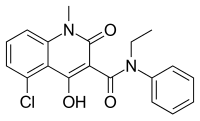
Ecopipam is a first-in-class drug that selectively blocks the actions of the neurotransmitter dopamine at its receptor. Dopamine receptors can be broadly classified into two families based on their structures: D1 receptors and D2 receptors. Ecopipam blocks dopamine only at D1 receptors, and thus acts differently than other commercially available medications. This mechanism explains why ecopipam is being tested as a potential treatment for stuttering.
The 10 patients selected for the clinical trial next month will undergo a physical examination and their medical history will be recorded. To ensure that their stuttering symptoms are sufficiently severe, their speech patterns will be analyzed by Professor Lisa LaSalle, a speech pathologist at the University of Redlands, and co-investigator on the study. Each patient will receive ecopipam for a limited time.
"We believe we could have results from our analysis in as soon as nine months," Maguire said. "A placebo-controlled clinical trial may then follow, pending approval. If ecopipam is found to be effective in controlling stuttering, we may have a viable solution for a disorder that can be traced back centuries."



 Midostaurin
Midostaurin 


 Topiramate
Topiramate  Levetiracetam
Levetiracetam