The combination of tenofovir disoproxil fumarate (TDF) and entecavir induces a high rate of viral suppression in patients with chronic hepatitis B virus (HBV) infection who have failed multiple nucleos(t)ide analogue (NA) regimens, phase IIIb results indicate.

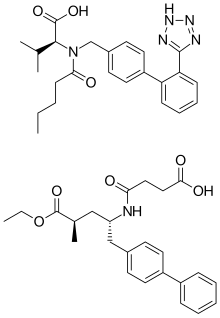
Entecavir Tenofovir disoproxil fumarate
The dual therapy could be "a highly effective option for difficult-to-treat multidrug-resistant" chronic HBV patients, the team writes in Liver International.
The 64 patients enrolled in this study had persistent viraemia, defined as serum HBV DNA levels above 60 IU/mL despite a minimum 24 weeks of rescue therapy, and documented genotypic resistance to one or more nucleoside analogue and a nucleotide analogue.
Treatment with TDF 300 mg and entecavir 1 mg once a day led to complete virological response (CVR), defined as HBV DNA levels under 60 IU/mL, in over half (56.3%) of the study population at 12 weeks. The CVR rate rose to 67.2% at week 24 and 85.9% at week 48.
The proportion of patients who achieved HBV DNA levels below 12 IU/mL, the lower limit of detection in this study, was 32.8%, 51.6% and 62.5% at weeks 12, 24 and 48, respectively.
The antiviral efficacy of the dual regimen was not affected by baseline viral load or the presence of baseline resistance mutations, report Sang Hoon Ahn (Yonsei University College of Medicine, Seoul, Republic of Korea) and fellow ESTEEM investigators.
However, a smaller proportion of participants with baseline triple resistance to lamivudine, adefovir and entecavir achieved CVR at week 48 relative to those with single or double resistance at baseline, at 67.7% versus rates ranging from 83.3% to 100.0%.
Virological breakthroughs occurred in five patients, but were transient in all cases and HBV DNA levels declined as treatment continued, say the researchers. And they add that none of the eight participants without CVR at week 48 had resistance mutations to TDF or any novel mutations.
TDF, entecavir duo 'highly effective' for difficult-to-treat chronic HBV: The combination of tenofovir disoproxil fumarate and entecavir induces a high rate of viral suppression in patients with chronic hepatitis B virus infection who have failed multiple nucleos(t)ide analogue regimens, phase IIIb results indicate.