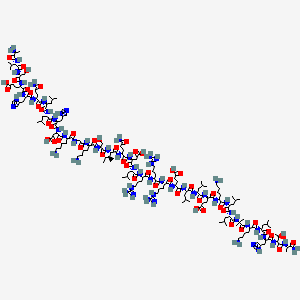
In continuation of my update on sacubitril and Valsartan
The fixed-dose combination of sacubitril and valsartan (trade name: Entresto) has been approved since November 2015 for adults with symptomatic chronic heart failure with reduced pump function (ejection fraction). The German Institute for Quality and Efficiency in Health Care (IQWiG) now examined in an early benefit assessment whether this drug combination offers an added benefit for patients in comparison with the appropriate comparator therapy.
According to the findings, the positive effects regarding mortality, necessity of heart failure hospitalizations, and quality of life predominate. These were not put into question by a negative effect in non-severe side effects; hence overall an indication of considerable added benefit can be derived from the data.
Approval study terminated prematurely
In its dossier, the drug manufacturer used data from a randomized controlled trial, which compared sacubitril/valsartan directly with enalapril, each in combination with a beta-blocker. Since a planned interim analysis was able to show after 51 months already that fewer cardiovascular deaths occurred under sacubitril/valsartan, the study was terminated prematurely.
Fewer deaths due to cardiovascular failure
The data from the dossier showed that all-cause mortality was lower under sacubitril/valsartan than under enalapril, which was mainly caused by fewer cardiovascular deaths.
The results regarding the frequency of hospitalizations due to heart failure were also in favour of the new fixed-dose combination; however, these were limited to patients with a lower severity grade (NYHA class I and II). Finally, the data on health-related quality of life also showed an advantage of sacubitril/valsartan.
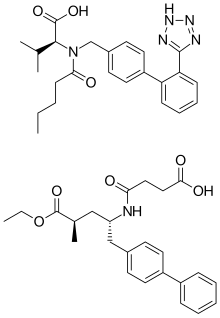
Entresto drug shows added benefit in symptomatic chronic heart failure: The fixed-dose combination of sacubitril and valsartan (trade name: Entresto) has been approved since November 2015 for adults with symptomatic chronic heart failure with reduced pump function (ejection fraction). The German Institute for Quality and Efficiency in Health Care (IQWiG) now examined in an early benefit assessment whether this drug combination offers an added benefit for patients in comparison with the appropriate comparator therapy.