In continuation of my update on lidocaine
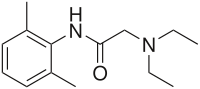
Sorrento Therapeutics, Inc. , received approval from the U.S. Food and Drug Administration (FDA) for ZTlido (lidocaine topical system) 1.8%. ZTlido is indicated for the relief of pain associated with post-herpetic neuralgia (PHN), also referred to as post-shingles pain. ZTlido is a major advancement in analgesics because of its proprietary adhesion technology demonstrating 12-hour wear with efficient lidocaine delivery, even during exercise.
“ZTlido was designed to solve a problem that is commonly reported with transdermal/topical patches: they don’t stay on. Based on the adhesion study results with ZTlido, we believe that ZTlido product will be welcomed by healthcare providers, patients and payers who are looking for an effective and efficient, local pain treatment,” said Dr. Henry Ji, Chairman and CEO of Sorrento and Scilex. “We also intend to explore the expansion of ZTlido into additional indications and the underlining platform technology of ZTlido for other active pharmaceutical ingredients (APIs) and combinations of APIs. As demonstrated by the NDA approval for ZTlido, our team successfully executed on our development plan for the product and now, looks forward to executing on our commercial and strategic alliance plans as well.”
“Topical lidocaine is an important option for healthcare providers to have in their armamentarium for treating PHN, a difficult-to-treat neuropathic pain,” stated Dr. Jeff Gudin, Director, Pain Management and Palliative Care, Englewood Hospital and Medical Center. “The Centers for Disease Control and Prevention’s guideline of non-opioid treatments for chronic pain recognizes topical lidocaine as an alternative first-line therapy. ZTlido now offers providers and patients this option.”
ZTlido’s anhydrous topical system is based on a novel technology that is designed to achieve superior adhesion and drug delivery efficiency. ZTlido only requires 36 mg/topical system versus 700 mg/patch of Lidoderm® (lidocaine patch 5%), the US reference product, to achieve the same therapeutic dose of drug. The safety and efficacy of ZTlido was bridged to Lidoderm in comparative pharmacokinetic studies that demonstrated bioequivalence between products.
According to an FDA report of the product quality of transdermal drug delivery systems, adhesion was the most widely reported quality defect of transdermal patches.¹ With a clear need for improved patch adhesion systems, ZTlido was specifically designed to maintain optimum skin contact throughout the 12-hour administration period. Adhesion is critical to the safety and efficacy quality of a topical system. Simply, the topical system must be in contact with skin to deliver the drug. ZTlido adhesion performance was demonstrated in a clinical study in fifty-four (54) healthy volunteers where forty-seven (47) subjects (87%) had adhesion scores of 0 (≥ 90% adhered; essentially no lift off the skin) for all evaluations performed every 3 hours during the 12 hours of administration, and seven (7) subjects (13%) had adhesion scores of 1 (≥ 75% to < 90% adhered; some edges only lifting off the skin) for at least one evaluation, and no subjects had scores of 2 or greater (< 75% adhered). In the same study 91% (49) of the subjects presented with a score of 0 at the end of the 12-hour administration period. The remaining 5 subjects had a score of 1.
In a separate Phase 1 comparative adhesion study in normal healthy subjects (n=44), ZTlido demonstrated superior adhesion (p <0.0001) to Lidoderm at 3 hours that improved over the 12-hour administration period.
According to recent IMS data, more than 100 million prescription lidocaine patches were sold in the US in 2017. Sorrento intends to have Scilex complete the final steps necessary to commercial launch of ZTlido in the US with the objective to make the product commercially available to patients sometime in 2018.


