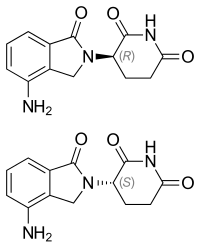
Celgene Corporation, announced the U.S. Food and Drug Administration (FDA) approved Revlimid (lenalidomide) in combination with a rituximab product (R²) for the treatment of adult patients with previously treated follicular lymphoma (FL) or marginal zone lymphoma (MZL) following Priority Review designation. This is the first FDA-approved combination treatment regimen for patients with these indolent forms of non-Hodgkin’s lymphoma (NHL) that does not include chemotherapy.
“Nearly 15 years following the initial FDA approval, Revlimid continues to demonstrate benefits for new patient populations,” said Jay Backstrom, M.D., M.P.H., Chief Medical Officer for Celgene. “Revlimid in combination with rituximab (R2) leads to immune-mediated treatment effects and represents a chemotherapy-free treatment option that can help patients with previously treated follicular lymphoma and marginal zone lymphoma delay disease progression.”
Immune dysfunction (meaning the immune system is not functioning optimally) is a defining aspect of indolent forms of NHL, including FL and MZL.1,2 When this dysfunction occurs, lymphocytes in the immune system either fail to detect or target cancerous cells.1,2
“Chemotherapy continues to be a standard of care for indolent forms of NHL, but most patients will relapse or become refractory to their current treatment,” said Meghan Gutierrez, Chief Executive Officer for the Lymphoma Research Foundation. “This approval represents a new therapeutic option for previously treated patients with follicular and marginal zone lymphomas, including those who relapse or no longer respond to initial treatment. We commend the patients and scientists who participated in the clinical study for advancing lymphoma research and treatment.”
The approval of R2 is based primarily on results from the randomized, double-blind, Phase 3 AUGMENT study, which evaluated the efficacy and safety of the R² combination versus rituximab plus placebo in patients with previously treated FL (n=295) and MZL (n=63).
In the AUGMENT study, treatment with R2 demonstrated a statistically significant improvement in the primary endpoint of progression-free survival (PFS), evaluated by an independent review committee, versus rituximab-placebo. The median PFS was 39.4 months for patients treated with R2 and 14.1 months for those treated with rituximab-placebo (HR: 0.46; 95% CI, 0.34-0.62; P<0.0001). Median follow-up time was 28.3 months (range, 0.1-51.3) in the intent to treat population (n=358). Although not statistically powered to detect a difference in overall survival, a numeric trend for improvement in overall survival (a secondary endpoint) was also seen with R2 versus rituximab-placebo (16 vs. 26 deaths) (HR: 0.61; 95% CI, 0.33-1.13).
Revlimid is only available through a restricted distribution program called Revlimid REMS® program. Revlimid has a boxed warning for embryo-fetal toxicity, hematologic toxicity, and venous and arterial thromboembolism. Adverse reactions reported in ≥15% of patients with FL/MZL treated with R2 were: neutropenia (58%), diarrhea (31%), constipation (26%), cough (24%), fatigue (22%), rash (22%), pyrexia (21%), leukopenia (20%), pruritus (20%), upper respiratory tract infections (18%), abdominal pain (18%), anemia (16%), headache (15%), thrombocytopenia (15%).
A Marketing Authorization Application for R2 is currently under review by the European Medicines Agency for the treatment of relapsed/refractory FL and MZL. A supplemental new drug application was also submitted to the Japanese Pharmaceuticals and Medical Devices Agency for an additional indication as well as dosage and administration updates for lenalidomide in combination with rituximab for the treatment of relapsed/refractory indolent B-cell NHL.