"Cardiovascular disease remains the leading cause of death of men and women globally and reduction of LDL cholesterol with statin medications has been demonstrated to substantially reduce the risk of first or recurrent cardiovascular events," said Dr. Gregg Fonarow, a professor of cardiology at the University of California, Los Angeles.
Friday, November 1, 2013
New Cholesterol-Lowering Drug, ALN-PCS Shows Early Promise
Thursday, April 15, 2010
Flaxseed lowers high cholesterol in men.....
Thursday, December 11, 2014
Cholesterol-fighting statins inhibit uterine fibroid tumors that account for 50% of hysterectomies...
Friday, November 20, 2009
Positive results from mipomersen- a new hope for FH sufferers...
Familial hypercholesterolemia (also spelled familial hypercholesterolaemia) is a genetic disorder characterized by high cholesterol levels, specifically very high low-density lipoprotein (LDL, "bad cholesterol") levels, in the blood and early cardiovascular disease. Many patients have mutations in the LDLR gene that encodes the LDL receptor protein, which normally removes LDL from the circulation, or apolipoprotein B (ApoB), which is the part of LDL that binds with the receptor; mutations in other genes are rare. Patients who have one abnormal copy (are heterozygous) of the LDLR gene may have premature cardiovascular disease at the age of 30 to 40. Having two abnormal copies (being homozygous) may cause severe cardiovascular disease in childhood. Heterozygous FH is a common genetic disorder, occurring in 1:500 people in most countries; homozygous FH is much rarer, occurring in 1 in a million births.
Heterozygous (FH) is normally treated with statins, bile acid sequestrants or other hypolipidemic agents that lower cholesterol levels. New cases are generally offered genetic counseling. Homozygous FH often does not respond to medical therapy and may require other treatments, including LDL apheresis (removal of LDL in a method similar to dialysis) and occasionally liver transplantation.
Recently, Genzyme Corp. and Isis Pharmaceuticals Inc have come up with some intresting results from the drug mipomersen [mipomersen - is an antisense oligonucleotide, with phosphorothioate linkage at 5'- postion and 2'-O-methoxymethyl moety] ( phase 3). As per the claim by the companies, the study met its primary endpoint in an intent-to-treat analysis, with a 25 percent reduction in LDL-cholesterol after 26 weeks of treatment, vs. 3 percent for placebo (p<0.001)>.
The trial met all of its secondary and tertiary endpoints, suggesting that mipomersen may offer potential benefits to patients beyond LDL-C reduction. Patients treated with mipomersen experienced a 27 percent reduction in apolipoprotein B vs. 3 percent for placebo; a 21 percent reduction in total cholesterol vs. 2 percent for placebo; and a 25 percent reduction in non-HDL cholesterol vs. 3 percent for placebo (all p<0.001).>Mipomersen patients’ HDL-C levels increased 15 percent (p=0.035 vs. placebo), which combined with the LDL-C reductions observed, resulted in improved LDL/HDL ratios, a ratio considered an important measure of cardiovascular risk. Mipomersen patients’ LDL/HDL ratios decreased by 34% (p<0.001>Mipomersen a representative of Isis’ leadership in the field of RNA targeted therapeutics will bring a sigh of relief to the sufferers of FH, in the days to come.
I had an opportunity to work with ISIS (as contract R & D, Innovasynth Technologies Limited, Khopoli) and really excited to see the results..
Ref : http://ir.isispharm.com/phoenix.zhtml?c=222170&p=irol-newsArticle&ID=1356364&highlight=
Thursday, January 7, 2016
Consuming tree nuts may reduce risk of cardiovascular disease, new study finds
Saturday, July 24, 2010
No Firm Conclusions About HDL Cholesterol Can Be Drawn from JUPITER Sub-Analysis
The European Society of Cardiology (ESC) is concerned that interpretations of a paper about cholesterol, published in the Lancet , could act to deter ongoing research efforts into developing new therapeutic strategies to increase high density lipoprotein (HDL) cholesterol. Caution, the ESC experts advise, should be displayed in the interpretation of the results.....
In the Lancet study, Paul Ridker and colleagues, from Brigham and Women's Hospital (Boston, MA, USA), undertook a retrospective post-hoc analysis of the JUPITER trial. The results show that if a normal, healthy individual has level of low density lipoprotein (LDL), known as "bad cholesterol", substantially lowered with a potent statin, then the level of HDL "good cholesterol" in that person no longer bears any relation to the remaining cardiovascular risk. More.....
Ref : http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2810%2960713-1/fulltext
Friday, June 17, 2016
Evolocumab could be more effective than ezetimibe in lowering cholesterol in statin-intolerant patients

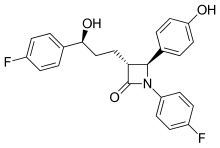
- In Phase A, patients were assigned to two groups. Each group was treated for 10 weeks with atorvastatin or placebo in a blinded fashion, then crossed over to the alternate therapy for another 10 weeks. Patients were asked to report any muscle pain or weakness.
- Patients who reported intolerable muscle symptoms on atorvastatin, but not placebo, moved to Phase B. In this 24-week phase, patients with confirmed statin intolerance were administered two alternative non-statin therapies, ezetimibe vs. evolocumab.
- The research is being presented at the American College of Cardiology's 65th Annual Scientific Session and simultaneously published online in the Journal of the American Medical Association."Statin intolerance has been a very challenging clinical problem," said Steven Nissen, M.D., chairman of Cardiovascular Medicine at Cleveland Clinic. "The study showed that PCSK9 inhibitors can significantly lower cholesterol in patients with documented statin intolerance, providing an effective treatment for these difficult to manage patients."The GAUSS-3 trial enrolled 511 patients with very high levels of LDL cholesterol - averaging more than 210 mg/dL ¬¬- and with a history of muscle-related statin intolerance. More than 80% of participants had previously reported intolerance to three or more statins. The study showed that 42.6 percent of these patients reported muscle pain or weakness on atorvastatin, but not placebo, and 26.5 percent on the placebo, but not atorvastatin.
Thursday, May 27, 2021
FDA Approves Roszet (rosuvastatin and ezetimibe) to Reduce LDL-C in Hyperlipidemia and Homozygous Familial Hypercholesterolemia
Althera Pharmaceuticals, a company focused on heart health, announced the FDA approval of Roszet (rosuvastatin and ezetimibe) tablets, as an adjunct to diet, for treatment of elevated low-density lipoprotein cholesterol (LDL-C) in adult patients with primary non-familial hyperlipidemia and in adult patients with homozygous familial hypercholesterolemia. Roszet contains rosuvastatin, a powerful statin for LDL-C reduction, and ezetimibe, an efficacious cholesterol absorption inhibitor. The two components work through distinct but complimentary mechanisms to give Roszet the power to significantly lower LDL-C.
“The optimal LDL-C levels in guidelines across the world have been shifting lower and now many patients need to get their LDL-C below 70 mg/dL,” said Dr. Christie Ballantyne, Chief of Cardiology and Cardiovascular Research at Baylor College of Medicine. “These levels can be quite difficult to achieve with just a statin on top of diet and exercise. Rosuvastatin and ezetimibe have been extensively studied in combination therapy and have been shown to significantly reduce LDL cholesterol beyond the statin alone. Combination therapy has been widely used in hypertension to achieve lower blood pressure targets. This new therapy provides a high efficacy statin plus ezetimibe in a single once daily pill which is a powerful new option to help get patients to the desirable LDL goal without increasing pill burden or requiring addition of injectable therapies”
"With Roszet’s approval in the U.S., we reaffirm our commitment to improving cholesterol treatment options for physicians and patients," said Sanjeev Agarwal, CEO of Althera Pharmaceuticals. "We are on a mission to positively impact patients’ health. By making this highly effective medicine available and affordable, we hope to improve the long-term health of patients, including those with prior cardiovascular disease.”
While a patient's out-of-pocket costs will vary depending on insurance status, the Roszet Savings Program aims to reduce co-pays to as little as $20 per month for eligible patients with commercial insurance coverage. Althera is continuing to work with all stakeholders to ensure that Roszet is affordable and accessible to all. Please visit http://www.roszet.com for more information and updates about the Roszet Savings Program and eligibility.
Roszet is available as a once-daily tablet with rosuvastatin/ezetimibe dosages of 5 mg/10 mg, 10 mg/10 mg, 20 mg/10 mg and 40 mg/10 mg.
https://en.wikipedia.org/wiki/Ezetimibe
https://en.wikipedia.org/wiki/Rosuvastatin
Thursday, January 3, 2013
FDA Approves Juxtapid - New Orphan Drug for Rare Cholesterol Disorder
FDA Approves Juxtapid - New Orphan Drug for Rare Cholesterol Disorder
Saturday, April 13, 2013
FDA Approves Juxtapid - New Orphan Drug for Rare Cholesterol Disorder
Monday, February 27, 2017
Is Avocado Good for Diabetes?
Diet and diabetes
How much avocado can people with diabetes eat?
Avocados and heart health
Fiber, blood sugar levels, and feeling full
Is Avocado Good for Diabetes?
Friday, October 21, 2011
New data on novel gene-silencing oligonucleotide technology...
In this study, Idera created 19mer GSOs for apolipoprotein B (ApoB) and proprotein convertase subtilisin/kexin type 9 (PCSK9) mRNA and evaluated their in vivo activity in mice following subcutaneous administration. The data demonstrate that treatment with each GSO led to a significant reduction in the concentration of the target associated mRNAs and protein. The effects were specific, with no significant effects being observed on ABCA1, ABCG1 or LXR mRNA levels. In addition, treatment with GSOs for either ApoB or PCSK9 resulted in a decrease in total serum cholesterol and LDL-cholesterol.
More...
Sunday, April 12, 2009
Niacin as one of the best and cheapest ways to manage cholesterol !

Niacin stimulates production of a vasodilator that dramatically increases blood flow to the face, causing the flush and the hot, prickly sensation - and beta-arrestin1 is the culprit that enables that to happen. However, beta-arrestin1 plays no role whatsoever in niacin's ability to lower cholesterol and fatty acids.
The finding reinforces some of Lefkowitz's (who has jointly worked with this group) recent research (that demonstrated that beta-arrestins which oftenly work in tandem with G proteins) can sometimes work independently of them and there by initiating their own signals.
The discovery opens the door to the possibility of developing a "biased ligand," a drug that would trigger GP109A, but not the beta-arrestins. Though further studies are essential in this regard, its a good beginning, as the research has achieved the first target i.e., to keep all the lipid-modifying benefits of niacin, but isolate its downside. Congrats Dr. Robert Walters et. al.,
Saturday, February 23, 2019
Psoriasis Meds Might Help Fight Heart Trouble, Too
"Classically a heart attack is caused by one of five risk factors: diabetes, hypertension, high cholesterol, family history or smoking," explained study lead researcher Dr. Nehal Mehta.
"Our study presents evidence that there is a sixth factor, inflammation," she said.
"The future of cardiovascular prevention may require a cholesterol reduction medication and an anti-inflammatory medication," said Dr. Guy Mintz, who directs heart health at Northwell Health's Sandra Atlas Bass Heart Hospital in Manhasset, N.Y.
"These are exciting times in the area of cardiovascular prevention," said Mintz, who wasn't involved with the study.
"This appears to be an anti-inflammatory effect," Mehta explained in an NHLBI news release. "In the absence of improvement in other cardiovascular risk factors, and without adding new cholesterol medications, patients' soft plaque still improved."
"The best statin in the world can only lower cardiovascular events by approximately 40 percent," Mintz pointed out. "So the question arises, what causes the other 60 percent of cardiovascular events?"
Sunday, November 13, 2016
Benefits of consuming dried fruits and nuts
Wednesday, April 4, 2012
Experimental Cholesterol Drug Could Be 'Game Changing'
Experimental Cholesterol Drug Could Be 'Game Changing': Experimental Cholesterol Drug Could Be 'Game Changing' [St.Joseph News-Press (Mo)] From St. Joseph News-Press (MO) (March 22, 2012) (CNN) -- A new, experimental cholesterol-fighting drug is creating quite a buzz among researchers and other...
Friday, November 9, 2012
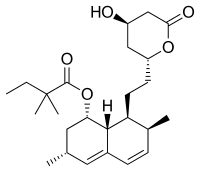
New medication lomitapide, shows promise as lipid-lowering therapy for rare cholesterol disorder
"The magnitude of this reduction in LDL-C and the fact that some patients reached or approached the LDL-C therapeutic goals is truly remarkable for this high risk population that historically doesn't respond to lipid-lowering drugs," said the study's lead author, Marina Cuchel, MD, PhD, research assistant professor of Medicine at Penn. "A reduction in LDL-C of this magnitude is certainly expected to favorably alter the clinical course of this devastating disease."
Tuesday, May 18, 2010
Individual's lifestyle choices can affect cholesterol, triglycerides levels: Mayo Clinic Health Letter
Sunday, January 6, 2013
Common cholesterol-lowering drug may help protect against cerebral malaria
"The molecular mechanisms that give rise to cerebral malaria and subsequent cognitive dysfunction are not yet known," says Zimmerman. "However, the fact that statin treatment decreases both injurious blood vessel inflammation and cognitive dysfunction suggests that a combination of vascular and inflammatory triggers leads to cerebral pathology and intellectual deficits."Ref : http://www.plospathogens.org/article/info%3Adoi%2F10.1371%2Fjournal.ppat.1003099
Common cholesterol-lowering drug may help protect against cerebral malaria
Friday, April 14, 2017
New research shows how cholesterol medicine has beneficial effect on immune defence system